Chapter: Clinical Anesthesiology: Anesthetic Management: Ambulatory, Non operating Room, & Office-Based Anesthesia
Anesthesia: Special Considerations in Out of the Operating Room Locations
SPECIAL CONSIDERATIONS IN OUT OF THE OPERATING ROOM LOCATIONS
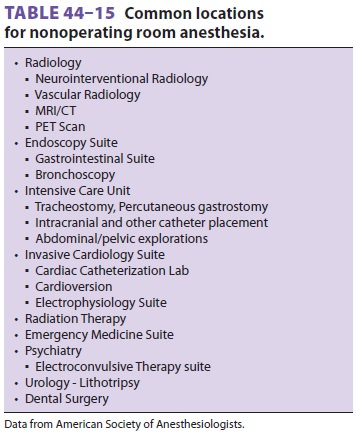
Anesthesia services are requested at various loca-tions throughout the
hospital facility; some of these are delineated in Table 44–15. As noted
through-out, routine anesthetic standards apply wherever the patient is
anesthetized. Out of the operating room patients often present with a wide
range of illnesses, unlike the elective patients gen-erally found in an
ambulatory setting. Furthermore,disposition postprocedure (whether discharge or
admission), needs appropriate coordination by the anesthesiologist for
postanesthesia care and/or safe transport from the remote unit.
Patients presenting to the gastrointestinal
endoscopy suite include healthy individuals for rou-tine diagnostic screenings,
as well as patients with fulminant cholangitis and sepsis or coexisting
dif-ficult airways. As always, the patient’s condition, as well as the specific
diagnostic/therapeutic pro-cedure, determines both the anesthetic techniques
(propofol deep sedation or general anesthesia vs. general anesthesia with LMA
or endotracheal tube) and the monitoring required.
General anesthesia is usually required in patients undergoing endoscopic
procedures for air-way and pulmonary pathology; an added complex-ity may
include the presence of a shared airway, and, in many patients, marginal
pulmonary status.
Patients undergoing cardiac catheterization
are routinely sedated by cardiologists without involvement of an anesthesiologist.
Occasionally, a patient with significant comorbidities, (eg, morbid obesity)
requires the presence of a qualified anes-thesia provider. General anesthesia
is often required for placement of aortic stents, which are increasingly being
performed by cardiologists in the cardiac cath-eterization laboratory.
Anesthesia staff should be prepared with arterial pressure monitoring and the
necessary vascular access to facilitate resuscitation, should emergent open
aneurysm repair be required.
Patients requiring electrophysiology
procedures for catheter-mediated arrhythmia ablation often need general
anesthesia. Such patients frequently have both systolic and diastolic heart
failure, leading to potential hemodynamic difficulties perioperatively. Sudden
hypotension can herald the development of pericardial tamponade secondary to
catheter perfo-ration of the heart. Other patients require sedation for the
placement of ICDs. Once placed, the device will be tested by inducing
ventricular fibrillation. During testing, deeper levels of sedation are
required, as the defibrillation shock can be frightening and very
uncomfortable. Likewise, anesthesia staff are called upon to provide anesthesia
for cardioversion of patients in atrial fibrillation. These patients usually have
associated cardiac diseases and require brief intravenous anesthetics to
facilitate cardioversion. Oftentimes, a transesophageal echocardiogram must be
performed prior to cardioversion to rule out clot in the left atrial appendage.
In such cases, anesthesia staff may also provide sedation for this procedure.
Determination as to whether a patient needs seda-tion or general anesthesia
with or without intubation is dependent upon routine patient assessment.
Children and some adults (ie, those that are claustrophobic,
developmentally disabled, or have conditions that prevent them to be still or
to lie flat) require anesthesia or sedation for MRI and computed tomography
(CT). Additionally, painful CT-guided biopsies may require anesthesia
man-agement. Anesthetic technique is dependent upon patient comorbidities.
MRI creates numerous problems for anesthe-sia
staff. First, all ferromagnetic materials must be excluded from the area of the
magnet. Most institu-tions have policies and training protocols to prevent
catastrophes (eg, oxygen tanks flying into the scan-ner). Second, all
anesthetic equipment must be compatible with the magnet in use. Third, patients
must be free of implants that could interact with the magnet, such as
pacemakers, vascular clips, ICDs, and infusion pumps. As with all out of the
operat-ing room anesthesia, the exact choice of technique is dependent upon the
patient’s comorbidities. Both deep sedation and general anesthesia approaches
with intubation or supraglottic airways can be used, depending on practitioner
preference and patient requirements.
Patients usually require general anesthesia
and tight blood pressure control to facilitate coiling and embolization of
cerebral aneurysms or arteriove-nous malformations. Patients taken to the radiology
suite for relief of portal hypertension via creation of a transjugular
intrahepatic portosystemic shunt (TIPS) are frequently hypovolemic, despite
profound ascites, and at risk of esophageal variceal bleeding and aspiration.
General anesthesia with intubation is preferred for management of the TIPS
procedure.
Anesthesia for electroconvulsive therapy is often provided in a separate
suite in the Psychiatry Unit or a monitored area in the hospital (eg, PACU).
Patient comorbidity, drug interactions with various psychotropic medications,
multiple anesthetic pro-cedures, and effects of anesthetic agents on the
qual-ity of electroconvulsive therapy also need to be taken into account.
Anesthesia staff are at times called to
provide anesthesia in the intensive care unit (ICU) for bed-side tracheostomy
or emergent chest and abdominal exploration in patients considered too
critically ill to tolerate transport to the operating room. In most of these
cases, the anesthesia staff generally employ ICU ventilator and monitors.
Intravenous agents are typically used along with muscle relaxants. When
performing anesthesia for bedside tracheostomy, it is important that the
endotracheal tube not be with-drawn from the trachea until end tidal CO 2 is mea-sured from the newly placed
tracheostomy tube.
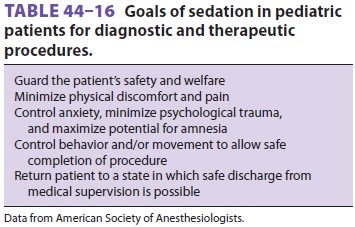
Pediatric patients deserve special mention;
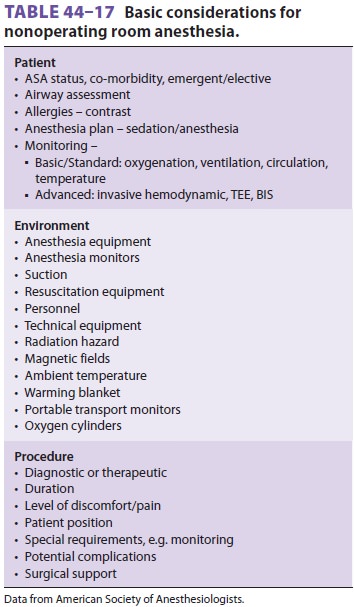
the (Table 44–16). Anesthesia
considerations for nonoperating room anesthesia are summarized in Table
44–17.
Related Topics