Chapter: Clinical Anesthesiology: Anesthetic Management: Ambulatory, Non operating Room, & Office-Based Anesthesia
Anesthesia: Non Operating Room Anesthesia
NON OPERATING ROOM ANESTHESIA
Off-site anesthesia (nonoperating room anesthe-sia) encompasses all sedation/anesthesia provided by anesthesiology services outside of the operat-ing room environment. Over the past few decades, requests for these services in remote locations have been steadily increasing, and in many large hospitals today more anesthetics are routinely administered for procedures off-site than in the operating room suite. According to some estimates, nonoperating room anesthesia accounts for 12.4% of all anes-thetic care in the United States. As a result, some clinical facilities have determined that is it safer and more cost-effective to assign anesthesia team(s) for scheduled blocks of times to provide care for such procedures, and some institutions are constructing procedural suites where bronchoscopy, gastrointes-tinal endoscopy, cardiac, and interventional radiol-ogy procedures can be performed in a centralized area for increased safety and efficiency. It is impor-tant to remember that the same basic standards for anesthesia care need to be met, regardless of the location. Furthermore, the challenges of unfamiliar environments that are far removed from the surgical suite, including anesthesia-naïve personnel, require advance planning for the off-site anesthesiologist.
Unlike patients undergoing office-based or
ambulatory surgery center procedures, out of the operating room patients are
frequently among the sickest of inpatients. Anesthesia staff are often called
to work in the gastrointestinal suite, cardiac cath-eterization laboratory,
electrophysiology laboratory, radiology suite, radiation oncology suite, and,
occa-sionally, the critical care unit. Often these locations were constructed
without anticipation that anesthe-sia would be provided there. Consequently,
anesthe-sia work space is routinely constrained, and access to the patient is
limited. Moreover, the procedure physicians and ancillary staff in these areas
often fail to understand what is required to safely deliver anesthesia (hence
the frequent request to “give them a squirt” of propofol) and do not know how
to assist
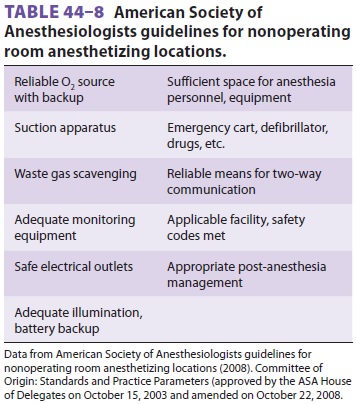
the anesthesia provider when difficulty arises. As noted in the ASA
guidelines, the expectations for out of the operating room anesthesia are the
same as in any practice location ( Table 44–8).
Basic principles for nonoperating room anes-thesia can be broadly
classified into three cat-egories: patient factors, environmental issues, and
procedure-related aspects. Patient factors include comorbidity, airway
assessment, fasting status, and monitoring. Environmental issues include anesthe-sia
equipment, emergency equipment, and magnetic and radiation hazards.
Procedure-related aspects include duration, level of discomfort, patient
posi-tion, and surgical support.
The ASA Closed Claims Database has dem-onstrated that claims related to
out of the operat-ing room anesthesia care have a greater severity of injury
than closed claims related to operating room anesthesia care. Monitored
anesthesia care was the primary technique in more than half of the claims
reviewed. Many of these closed claims arose from injuries related to inadequate
oxygenation/ventila-tion during procedures in the gastrointestinal suite.
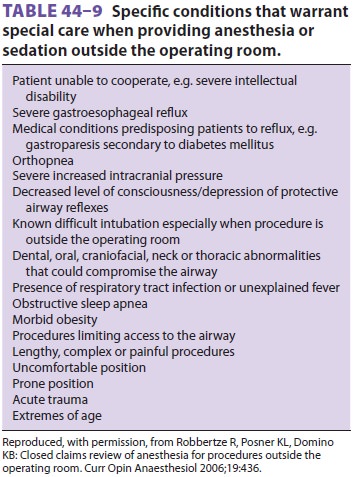
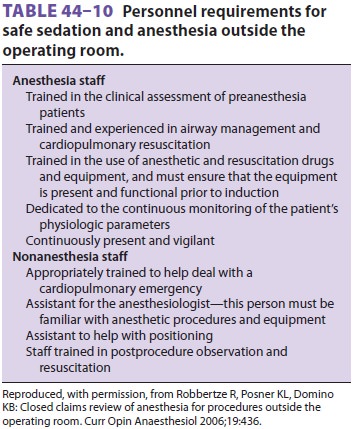
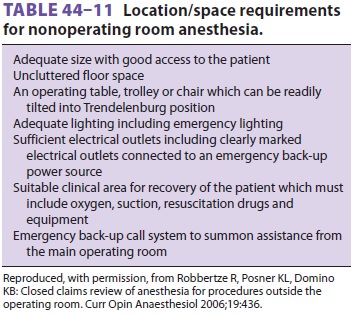
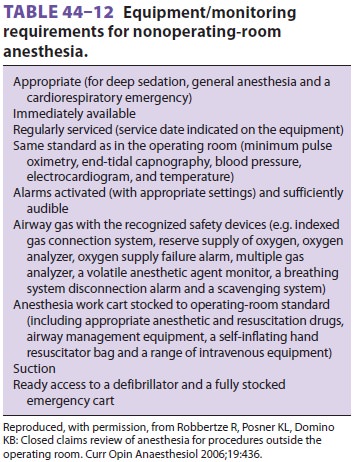
Suggested requirements for the safe delivery of out of the operating room
anesthesia are presented in Tables 44–9, 44–10, 44–11, and 44–12.
Increasingly, nonanesthesia providers in the
gastrointestinal lab and the emergency department provide sedation with a variety
of agents, including propofol and ketamine. In fact, some reports indi-cate
that nonanesthesia providers provide admin-ister sedation and analgesia for
almost 40% of the procedures performed in the United States. The ASA guidelines
and the Joint Commission have described the continuum of depth of sedation,
rang-ing from minimal sedation to general anesthesia (Table
44–13). Recently, the Centers for Medicare and
Medicaid Services has mandated that all sedation in a hospital be under the
direction of a physician— generally, the anesthesia service chief.
Consequently, anesthesiologists must not only from time to time
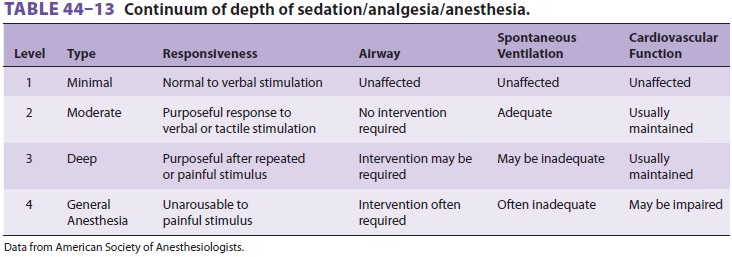
provide anesthesia in a nonoperating room setting, but must also develop
policies and quality assurance review mechanisms for nonanesthesia providers to
safely provide sedation. Such policies should be focused on assuring that the
“sedationist” has the necessary skills to provide for patient rescue, should
mild or moderate sedation become deep sedation or general anesthesia.
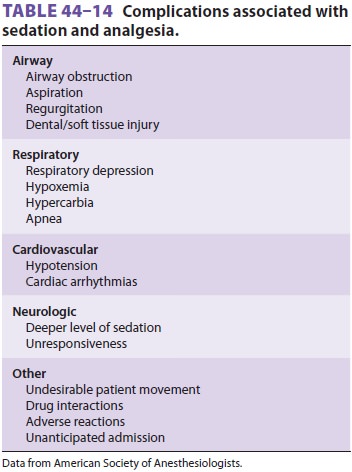
Risks associated with sedation/analgesia are highlighted in Table
44–14. Sedation providers should know how to reverse benzodiazepines and
opioids and provide bag/mask airway support and to be facile in the use of
airway adjuvants. A mecha-nism to ensure the timely arrival of anesthesia
per-sonnel capable of airway rescue must likewise be incorporated into such
policies.
Related Topics