Chapter: Obstetrics and Gynecology: Amenorrhea and Abnormal Uterine Bleeding
Abnormal Uterine Bleeding
ABNORMAL UTERINE BLEEDING
Failure to ovulate results in
either amenorrhea or irregu-lar uterine bleeding. Irregular bleeding that is
unrelated to anatomic lesions of the uterus is referred to as anovula-tory uterine bleeding. It is
most likely to occur in asso-ciation with anovulation as found in polycystic
ovarian disease, exogenous obesity, or adrenal hyperplasia.
Women
with hypothalamic amenorrhea (hypothalamic– pituitary dysfunction) and no
genital tract obstruction are in a state of estrogen deficiency. Estrogen
is inadequate to stimulategrowth and development of the endometrium. Therefore,
there is inadequate endometrium for uterine bleeding to occur. In contrast, women with oligo-ovulation and
anovulationwith abnormal uterine bleeding have constant, noncyclic blood
estrogen concentrations that stimulate growth and development of the
endometrium. Without the predictable effect of
ovulation,progesterone-induced changes do not occur. Initially, these patients
have amenorrhea because of the chronic, constant estrogen levels but,
eventually, the endometrium outgrows its blood supply and sloughs from the
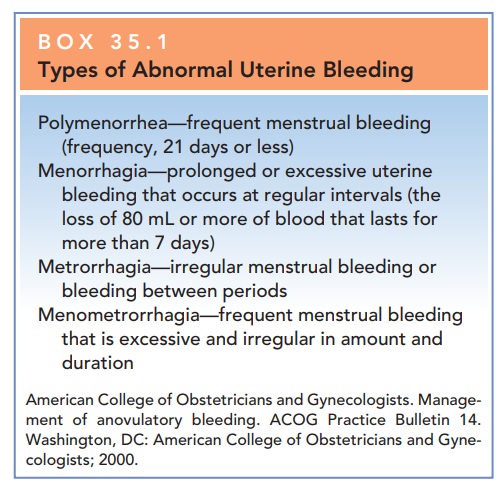
uterus at irregular times and in unpredictable amounts (see Box 35.1).
When there is chronic stimulation
of the endometrium from low plasma concentrations of estrogens, the episodes of
uterine bleeding are infrequent and light. Alternatively, with chronic
stimulation of the endometrium from increased plasma concentrations of
estrogens, the episodes of uterine bleeding can be frequent and heavy. Because
amenorrhea and abnormal uterine bleeding both result from anovulation, it is
not surprising that they can occur at different times in the same patient.
Subtle alterations in the
mechanisms of ovulation can produce abnormal cycles, even when ovulation occurs
(e.g., the luteal phase defect). In the luteal
phase defect, ovulation does occur; however, the corpus luteum of the ovary
is not fully developed to secrete adequate quantities of progesterone to
support the endometrium for the usual 13 to 14 days and is not adequate to
support a pregnancy if conception does occur. The menstrual cycle is shortened,
and menstruation occurs earlier than expected. Although this is not classical
anovulatory uterine bleeding, it is con-sidered to be in the same category.
Another example is mid-cycle spotting, in which patients report bleeding at the
time of ovulation. In the absence of demonstrable pathology, this self-limited
bleeding can be attributed to the sudden drop in estrogen level that occurs at
this time of the cycle.
Diagnosis of Abnormal Uterine Bleeding
Diagnosis of abnormal uterine
bleeding should be sus-pected when vaginal bleeding is not regular, not
pre-dictable, and not associated with premenstrual signs and symptoms that
usually accompany ovulatory cycles. These signs and symptoms include breast
fullness, abdominal bloating, mood changes, edema, weight gain, and uterine
cramps.
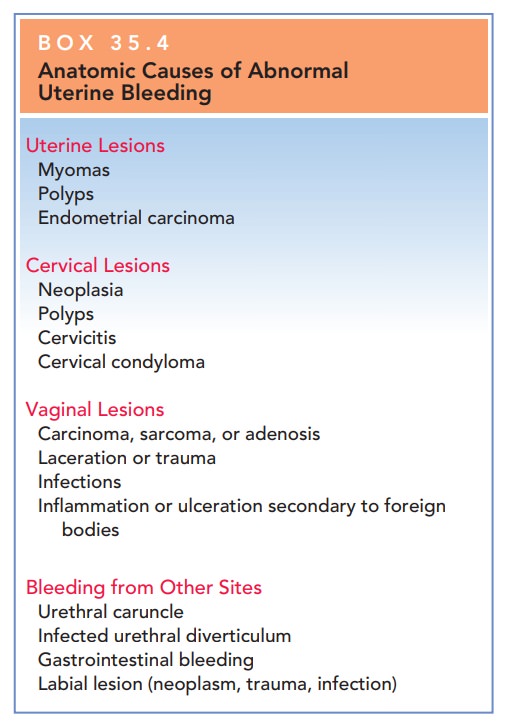
Before
anovulatory uterine bleeding can be diagnosed, anatomic causes including
neoplasia should be excluded.
In a reproductive-aged woman,
complications of pregnancy as a cause of irregular vaginal bleeding should be
excluded. Other anatomic causes of irregular vaginal bleeding include uterine
leiomyomata, inflammation or infection of the gen-ital tract, hyperplasia or
carcinoma of the cervix or endo-metrium, cervical and endometrial polyps, and
lesions of the vagina (Box 35.4). Pelvic ultrasonography or sonohysterog-raphy
may assist in diagnosing these lesions. Women with organic causes for bleeding
may have regular ovulatory cycles with superimposed irregular bleeding.
If the diagnosis is uncertain
based on history and phys-ical examination alone, a woman may keep a basal body
temperature chart for 6 to 8 weeks to look for the shift in the basal
temperature that occurs with ovulation. An ovu-lation predictor kit may also be
used. Luteal phase pro-gestin may also be measured. In cases of anovulation and
abnormal bleeding, an endometrial biopsy may reveal endometrial hyperplasia.
Because abnormal uterine bleed-ing results from chronic, unopposed estrogenic
stimulation of the endometrium, the endometrium appears prolifera-tive or, with
prolonged estrogenic stimulation, hyperplas-tic. Without treatment, these women
are at increased risk for endometrial cancer.
Treatment of Abnormal Uterine Bleeding
The risks to a woman with anovulatory
uterine bleeding include anemia, incapacitating blood loss, endometrial
hyperplasia, and carcinoma. Uterine bleeding can be severe enough to require
hospitalization. Both hemor rhage and endometrial hyperplasia can be prevented
by appropriate management.
Box 35.4
Anatomic Causes of Abnormal Uterine Bleeding
Uterine Lesions
Myomas
Polyps
Endometrial
carcinoma
Cervical Lesions
Neoplasia
Polyps
Cervicitis
Cervical
condyloma
Vaginal Lesions
Carcinoma,
sarcoma, or adenosis
Laceration
or trauma
Infections
Inflammation
or ulceration secondary to foreign bodies
Bleeding from Other Sites
Urethral
caruncle
Infected
urethral diverticulum
Gastrointestinal
bleeding
Labial
lesion (neoplasm, trauma, infection)
The
primary goal of treatment of anovulatory uterine bleed-ing is to ensure regular
shedding of the endometrium and conse-quent regulation of uterine bleeding. If
ovulation is achieved,conversion of the proliferative endometrium into
secretory endometrium will result in predictable uterine withdrawal bleeding.
A progestational agent may be
administered for a mini-mum of 10 days. The most commonly used agent is
me-droxyprogesterone acetate. When the progestational agent is discontinued,
uterine withdrawal bleeding ensues, thereby mimicking physiologic withdrawal of
progesterone.
As an alternative, administration
of oral contraceptives suppresses the endometrium and establishes regular,
pre-dictable withdrawal cycles. No particular oral contraceptive preparation is
better than any of the others for this purpose. Women who take oral
contraceptives as treatment of abnormal uterine bleeding often resume abnormal
uterine bleeding after therapy is discontinued.
If a patient is being treated for
a particularly heavy bleeding episode, once organic pathology has been ruled
out, treatment should focus on two issues: (1) control of the acute episode,
and (2) prevention of future recurrences. Both high-dose estrogen and progestin
therapy as well as combination treatment (oral contraceptive pills, four per
day) have been advocated for management of heavy abnor-mal bleeding in the
acute phase. Long-term preventive management may include either intermittent
progestin treatment or oral contraceptives. Uterine bleeding that does not
respond to medical therapy often is managed sur-gically with endometrial
ablation or hysterectomy. Before proceeding with endometrial ablation, one must
rule out endometrial carcinoma.
Related Topics