Chapter: Medical Physiology: Dominant Role of the Kidney in Long-Term Regulation of Arterial Pressure and in Hypertension: The Integrated System for Pressure Control
тАЬPrimary (Essential) HypertensionтАЭ
тАЬPrimary (Essential) HypertensionтАЭ
About 90 to 95 per cent of all people who have hyper-tension are said to have тАЬprimary hypertension,тАЭ also widely known as тАЬessential hypertensionтАЭ by many clinicians. These terms mean simply that the hypertensionis of unknown origin, in contrast to those forms ofhypertension that are secondary to known causes, such as renal artery stenosis. In some patients with primary hypertension, there is a strong hereditary tendency, the same as occurs in animal strains of genetic hyperten-sion discussed above.
In most patients, excess weight gain and sedentarylifestyle appear to play a major role in causing hyper-tension. The majority of patients with hypertension are overweight, and studies of different populations suggest that excess weight gain and obesity may account for as much as 65 to 70 percent of the risk for developing primary hypertension. Clinical studies have clearly shown the value of weight loss for reduc-ing blood pressure in most patients with hypertension. In fact, new clinical guidelines for treating hyper-tension recommend increased physical activity and weight loss as a first step in treating most patients with hypertension.
Some of the characteristics of primary hypertension caused by excess weight gain and obesity include:
1. Cardiac output is increased due, in part, to theadditional blood flow required for the extra adipose tissue. However, blood flow in the heart, kidneys, gastrointestinal tract, and skeletal muscle also increases with weight gain due to increased metabolic rate and growth of the organs and tissues in response to their increased metabolic demands. As the hypertension is sustained for many months and years, total peripheral vascular resistance may be increased.
2. Sympathetic nerve activity, especially in the kidneys, is increased in overweight patients. The causes ofincreased sympathetic activity in obesity are not fully understood, but recent studies suggest that hormones, such as leptin, released from fat cells may directly stimulate multiple regions of the hypothalamus, which, in turn, have an excitatory influence on the vasomotor centers of the brain medulla.
3. Angiotensin II and aldosterone levels are increased two- to threefold in many obese patients. This maybe caused partly by increased sympathetic nerve stimulation, which increases renin release by the kidneys and therefore formation of angiotensin II, which, in turn, stimulates the adrenal gland to secrete aldosterone.
4. The renal-pressure natriuresis mechanism is impaired, and the kidneys will not excrete adequate amounts of salt and water unless the arterial pressure is high or unless kidney function is somehow improved. In other words, if the meanarterial pressure in the essential hypertensive person is 150 mm Hg, acute reduction of the mean arterial pressure artificially to the normal value of 100 mm Hg (but without otherwise altering renal function except for the decreased pressure) will cause almost total anuria, and the person will retain salt and water until the pressure rises back to the elevated value of 150 mm Hg. Chronic reductions in arterial pressure with effective antihypertensive therapies, however, usually do not cause marked salt and water retention by the kidneys because these therapies also improve renal-pressure natriuresis, as discussed below.
Experimental studies in obese animals and obese patients suggest that impaired renal-pressure natri-uresis in obesity hypertension is caused mainly by increased renal tubular reabsorption of salt and water due to increased sympathetic nerve activity and increased levels of angiotensin II and aldosterone. However, if hypertension is not effectively treated, there may also be vascular damage in the kidneys that can reduce the glomerular filtration rate and increase the severity of the hypertension. Eventually uncon-trolled hypertension associated with obesity can lead to severe vascular injury and complete loss of kidney function.
Graphical Analysis of Arterial Pressure Control in Essential Hypertension. Figure 19тАУ14 is a graphical analysis ofessential hypertension. The curves of this figure are called sodium-loading renal function curves because the arterial pressure in each instance is increased very slowly, over many days or weeks, by gradually
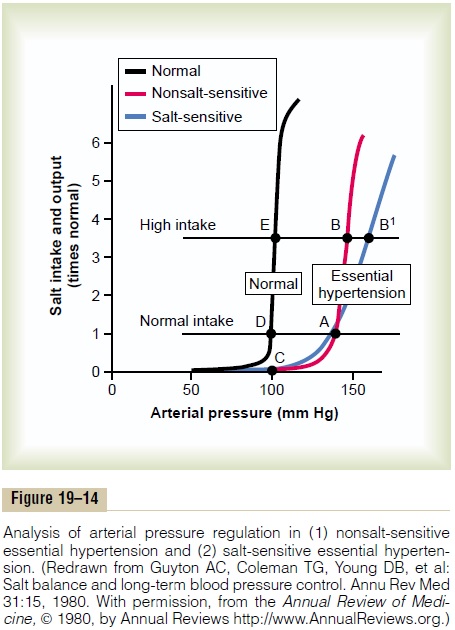
increasing the level of sodium intake. The sodium-loading type of curve can be determined by increasing the level of sodium intake to a new level every few days, then waiting for the renal output of sodium to come into balance with the intake, and at the same time recording the changes in arterial pressure.
When this procedure is used in essential hyperten-sive patients, two types of curves, shown to the right in Figure 19тАУ14, can be recorded in essential hyperten-sive patients, one called (1) nonsalt-sensitive hyperten-sion and the other (2) salt-sensitivehypertension. Note in both instances that the curves are shifted to the right, to a much higher pressure level than for normal people. Now, let us plot on this same graph (1) a normal level of salt intake and (2) a high level of salt intake representing 3.5 times the normal intake. In the case of the person with nonsalt-sensitive essential hypertension, the arterial pressure does not increase significantly when changing from normal salt intake to high salt intake. Conversely, in those patients who have salt-sensitive essential hypertension, the high salt intake significantly exacerbates the hypertension.
Two additional points should be emphasized: (1) Salt-sensitivity of blood pressure is not an all-or-none characteristicтАФit is a quantitative characteristic, with some individuals being more salt-sensitive than others.
(2) Salt-sensitivity of blood pressure is not a fixed characteristic; instead, blood pressure usually becomes more salt-sensitive as a person ages, especially after 50 or 60 years of age.
The reason for the difference between nonsalt-sensitive essential hypertension and salt-sensitive hypertension is presumably related to structural or functional differences in the kidneys of these two types of hypertensive patients. For example, salt-sensitive hypertension may occur with different types of chronic renal disease due to gradual loss of the functional units of the kidneys (the nephrons) or to normal aging. Abnormal function of the renin-angiotensin system can also cause blood pres-sure to become salt-sensitive.
Treatment of Essential Hypertension. Current guidelinesfor treating hypertension recommend, as a first step, lifestyle modifications that are aimed at increasing physical activity and weight loss in most patients. Unfortunately, many patients are unable to lose weight, and pharmacological treatment with antihy-pertensive drugs must be initiated.
Two general classes of drugs are used to treat hyper-tension: (1) vasodilator drugs that increase renal blood flow and (2) natriuretic or diuretic drugs that decrease tubular reabsorption of salt and water.
Vasodilator drugs usually cause vasodilation in many other tissues of the body as well as in the kidneys. Different ones act in one of the following ways: (1) by inhibiting sympathetic nervous signals to the kidneys or by blocking the action of the sympa-thetic transmitter substance on the renal vasculature, (2) by directly relaxing the smooth muscle of the renal vasculature, or (3) by blocking the action of the renin-angiotensin system on the renal vasculature or renal tubules.
Those drugs that reduce reabsorption of salt and water by the renal tubules include especially drugs that block active transport of sodium through the tubular wall; this blockage in turn also prevents the reabsorp-tion of water..
Related Topics