Chapter: Essentials of Psychiatry: Childhood Disorders: Tic Disorders
Treatment of Cooccurring Psychiatric Disorders in TouretteŌĆÖs Disorder
Treatment of Cooccurring
Psychiatric Disorders in TouretteŌĆÖs Disorder
Treatment of Attention-deficit/Hyperactivity Disorder
Nonpharmacological Approaches
The nonpharmacological approaches to ADHD in
TouretteŌĆÖs disorder are similar to approaches in children without TouretteŌĆÖs
disorder. The presence both at home and at school of a structured environment,
consistent behavioral management, and a gener-ally positive, rewarding
atmosphere can produce significant im-provement in ADHD symptoms. Increasingly,
there are specific programs for children with ADHD that go beyond basic
positive programming and include more intensive and specific behavioral
approaches.
Pharmacological Treatments
The two major difficulties in the treatment of ADHD
in TouretteŌĆÖs disorder are the risk of side effects from the stimulants and
desipramine, arguably the most potent treatment agents for ADHD and the lack of
adequate alternatives.
Stimulants
In the early 1970s, a number of reports of
induction or exacerbation of tics by stimulant medications raised concerns
about the role of stimulants as a cause of TouretteŌĆÖs disorder. At that time,
the con-cern was that stimulants could be causing tics de novo or that in-creases in tic severity would endure even if
stimulant medications were discontinued. Concurrent with these reports, other
authors noted that tic induction or exacerbation was relatively infrequent and
that the beneficial effects in some patients with TouretteŌĆÖs dis-order
outweighed any negative impact on tic severity.
As a result, stimulants have been used infrequently
for ADHD in TouretteŌĆÖs disorder. However, results of short-term and long-term
double-blind, placebo-controlled trials with stimulants in TouretteŌĆÖs disorder
are positive and support a role for stimu-lants in some patients with
TouretteŌĆÖs disorder plus ADHD. In-creasingly, psychiatrists are cautiously, and
with fully informed consent, using stimulant medication in selected children
and adolescents with TouretteŌĆÖs disorder and ADHD. In the patient in whom tics
are increased by stimulants, combined treatment with stimulants and
tic-suppressing agents can be used.
More recently, in a large (N 5 136) multicenter double-blind, placebo-controlled
trial, children with ADHD and a chronic tic disorder were randomly assigned to
clonidine alone, methylphenidate alone, clonidine plus methylphenidate or
placebo for the treatment of their ADHD. The results suggest that the active
treatments were superior to placebo, with the combination treatment being the
most effective. With respect to worsening of tic severity the percentage of
children with worsening of tics was similar in each of the medication
conditions including placebo. For methylphenidate, 20% reported tic increases
compared with 26% on clonidine alone and 22% on placebo. Interestingly tic
severity lessened in all active treatment groups even in the methylphenidate
group. Other side effects were predictable with sedation commonly associated
with clonidine treatment (The Tourette Syndrome Study Group, 2002). Given the
controversy regarding the coadministration of clonidine and methylphenidate it
is important to note the absence of cardiac toxicity in children on combined medication.
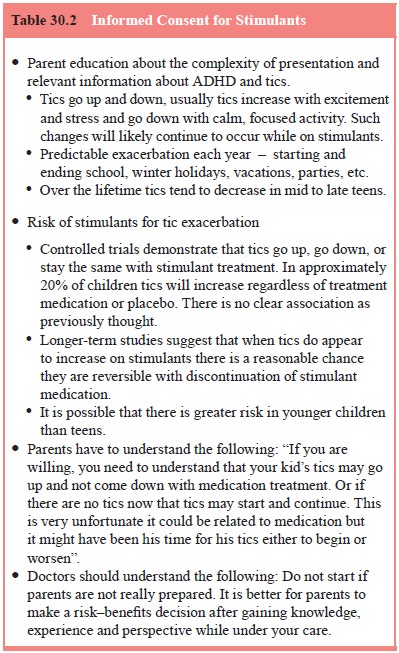
Given the above, informed consent prior to
initiating stim-ulant medication should include information regarding the risks
for new onset of tics or tic exacerbations. In Table 30.2 is a listing of
topics that might be useful to address during informed consent. This listing is
not intended to be a comprehensive or exhaustive.
Desipramine
Desipramine is a TCA with prominent noradrenergic activity that has been noted to improve attention and concentration in children and adolescents with ADHD and TouretteŌĆÖs disorder plus ADHD. Symptom improvement is often significant with lower doses than needed for depression. Side effects are generally limited. The cardiac side effects of increased heart rate and elevation in blood pressure are usually not clinically significant; however, reports of sudden death in children and adolescents taking desipramine have resulted in marked reductions nationally in the use of desipramine in children and adolescents.
Nortriptyline
Given the concern about the cardiac effects of
desipramine, TCAs such as nortriptyline have been used for the treatment of
ADHD. The only available report, a chart review, assessed the effect of
nortriptyline in children and adolescents with TouretteŌĆÖs disorder plus ADHD.
The majority of subjects experienced mod-erate to marked improvement in both
ADHD and tics (Wilens et al., 1993).
Although the concern regarding sudden death is less with nortriptyline than with desipramine, it is prudent to obtain
baseline and follow-up electrocardiograms.
Clonidine and Guanfacine
Data supporting the efficacy of these agents has
been limited to open trial or small controlled trials. In the largest trial to
date subjects (N 5 34; mean
age of 10.4 years) were randomly assigned to 8 weeks of guanfacine or placebo.
Guanfacine was superior to placebo (37 versus 8%) in reduction of the total
score on the teacher-rated ADHD Rating Scale and significant differences were
also observed in omission and commission errors on a continuous performance
test (Scahill et al., 2001).
Selective Noradrenergic Reuptake Inhibitors (SNRIs)
One SNRI has recently been approved for the
treatment of ADHD in children and one is under FDA review for major depression.
Atomoxetine has been demonstrated to be effective and approved for use in
children and adults with ADHD. Given its mechanism of action it is possible
that atomoxetine could improve ADHD symptoms without exacerbating tic symptoms.
Studies are cur-rently underway. Similarly reboxetine, which has an indication
in Europe for depression, may be useful for ADHD in people with tics disorders.
Treatment of ObsessiveŌĆōCompulsive Disorder
Nonpharmacological Approaches
The positive role of cognitiveŌĆōbehavioral
treatments of OCD is well established in adults. Most reports of
nonpharmacological treatment of OCD in children and adolescents are case
studies. Only one report has a sufficient sample size and a protocol-driven,
cognitiveŌĆōbehavioral treatment regimen to begin to establish the possible role
of such treatment in children and adolescents with OCD. There are no specific
reports of cognitiveŌĆōbehavioral treatment or other nonpharmacological
treatments of OCD in adults or children with TouretteŌĆÖs disorder. Given the
success of cognitiveŌĆōbehavioral treatment in OCD, it is likely that patients
with TouretteŌĆÖs disorder and OCD will also be able to benefit from
cognitiveŌĆōbehavioral treatment.
Pharmacological Treatments
The number of agents available for the treatment of
OCD in pa-tients with and without TouretteŌĆÖs disorder is increasing. Cur-rently
available agents include the TCA clomipramine and the specific serotonin
reuptake inhibitors fluoxetine, sertraline, par-oxetine, fluvoxamine and
citalopram. Even though only a few of these agents have a specific indication
for OCD (clomipramine and fluvoxamine), others may be effective in OCD given
their serotoninergic activity. The choice of agent depends on the side-effect profile,
the potential drug interactions and the psychia-tristŌĆÖs familiarity with the
drug.
With the exception of clomipramine, all of the
available agents have mild and somewhat similar side-effect profiles. Drug
interaction issues must be taken into account, especially in chil-dren with
complex presentations or multiple medical conditions given the increased
possibility of multiple drug regimens. The re-ports of elevated TCA levels in
patients receiving TCA and fluox-etine are good examples of unforeseen drug
interactions with the specific serotonin reuptake inhibitors.
Increasingly, augmentation strategies are pursued
in pa-tients with OCD and with TouretteŌĆÖs disorder plus OCD, when clinical
symptoms remain after initial treatment. A number of strategies have been used,
including augmentation with lithium, neuroleptics, buspirone, clonazepam,
liothyronine sodium (T3) and fenfluramine. Although positive outcomes of these
strate-gies have been reported in open trials, only neuroleptic aug-mentation
has shown to be of any benefit in controlled trials. Interestingly, controlled
trials of haloperidol combined with specific serotonin reuptake inhibitors in
patients with TouretteŌĆÖs disorder and OCD demonstrated improvement in both tic
and OCD symptoms.
Treatment-refractory Cases
Strategies for approaching two types of
treatment-refractory symptoms are discussed here: 1) patients who are truly
treatment-refractory with severe and impairing symptoms of TouretteŌĆÖs disorder
and OCD, despite conventional and heroic treatments, and 2) patients, often
children, who are clinically complex and enigmatic, and whose impairment is
disproportionally greater than their tic, obsessiveŌĆōcompulsive, or ADHD
symptoms would suggest.
Treatment-refractory Tics
Perhaps the most important ŌĆ£treatmentŌĆØ in patients
with severe incapacitating tics is a full clinical reevaluation to assess the
ad-equacy of previous evaluations and treatment efforts. It is not un-common
for treatment-refractory patients to have had inadequate evaluations and
treatment trials.
Two alternative treatment strategies are available
for truly treatment-refractory tics. When a single tic or a few tics are
re-fractory and impairing, the injection of botulinum toxin into the specific
muscle group can be helpful. This strategy is most useful for painful, dystonic
tics. Treatment has a long duration of action, but the effect does decrease in
2 to 4 months, and repeated injec-tions may be necessary. Specific side effects
are few, other than weakness in the affected muscle. Some patients reported the
loss of the premonitory sensation with their botulinum toxin treat-ment. For
the psychiatrist, it is essential to work with a neurolo-gist experienced in
using botulinum toxin.
There have been reports in the literature and the
media concerning the use of neurosurgical approaches for the treat-ment of
refractory tics. To date, the optimal size and location of the surgical
treatment lesions are not known. There are no well-controlled trials, although
some data are available from patients with OCD and tics who were treated for
OCD. In these patients, the impact on tic severity was mixed. Because these
approaches are particularly controversial, it is important, before considering
neurosurgical approaches, to complete a detailed and exhaustive reevaluation to
determine whether all other treatment options are exhausted. It is also
important that patients who pursue neuro-surgical approaches consider centers
of clinical excellence where controlled treatment trials are ongoing.
Treatment-refractory ObsessiveŌĆō Compulsive Disorder
A similarly thorough and exhaustive reevaluation is
critical for patients with TouretteŌĆÖs disorder plus OCD who present as
treat-ment-refractory. Diagnostic reevaluation focuses on whether other
psychiatric disorders are present and disabling and whether the current
hierarchy of clinical disability considers all conditions.
Pharmacological reevaluation is especially critical
be-cause there are an increasing number of new medications and potential
medication combinations. Rather than repeated change from one antiobsessional
agent to another, consideration can be given to augmentation strategies,
because they take less time than changing agents and may offer synergistic
benefits. Low-dose neuroleptic augmentation is the best first choice;
controlled trials support the use of low-dose neuroleptics for augmentation of
serotonin reuptake inhibitors in OCD. Lithium and T3 are proven, effective
augmenters of antidepressants for depression, yet neither is proven effective
in OCD. Because of the frequent overlap of OCD and major depression, lithium or
T3 augmenta-tion may be the next best choice.
Treatment-refractory or malignant OCD has been the
psy-chiatric disorder most frequently treated with neurosurgical in-terventions
in the modern era. Whereas it is a major treatment in-tervention, the surgical
approaches are somewhat better defined, and the outcome in severe cases is
often positive. Also, medical centers are available that specialize in the
presurgical work-up and the neurosurgical procedure.
Clinically Complex Patients
Clinically complex patients may be severely
impaired without having severe tic or OCD symptoms. The clinically complex
patient is often a diagnostic dilemma with additional diagnoses complicating
the clinical picture. In addition, patients can be-come clinically complex when
otherwise straightforward treat-ments are a challenge to implement.
Diagnosis
In clinically complex patients, the diagnostic
challenge is not an accurate assessment of tics, ADHD, obsessiveŌĆōcompulsive
symptoms, or LDs, although this is important. In clinically com-plex patients,
the diagnostic goal is to identify what other condi-tions or factors may be
present that make the current treatment approaches difficult.
From a strictly diagnostic point of view, it is the
additional psychiatric conditions beyond TouretteŌĆÖs disorder, OCD, ADHD and LDs
that often escape clinical observation and result in diag-nostic dilemmas and
treatment failures.
Treatment Implementation
Clinical problems occur when the treating
psychiatrist does not have access to critical information or is not in control
of the treat-ment process. Traditionally, psychiatrists develop a relationship
with the patient and the other major figures in the patientŌĆÖs life. Given the
current clinical climate, a comprehensive level of in-volvement can be
overwhelming and enormously time-consum-ing for the psychiatrist. Because it is
increasingly difficult for the psychiatrist to be as involved as necessary,
problems with poorly coordinated team efforts and the psychiatristŌĆÖs lack of
awareness of important clinical issues can have a negative impact on the
treatment of a patient.
Psychiatrists who work with children and
adolescents may wish to consider changes in their treatment approaches to these
patients. Experience in tertiary care centers suggests that expanded time with
the parents is a critically important and ef-ficient approach to care.
Psychiatrists who form a treatment part-nership with families, respecting and
addressing their concerns, educating them about TouretteŌĆÖs disorder, training
them to evalu-ate and manage complex behaviors, and empowering them to be an
effective advocate for their child, are providing good care. In working
directly with families, the collection of important infor-mation regarding the
familyŌĆÖs and patientŌĆÖs functioning is direct and regular, and often small
interventions can produce changes in family functioning that have a positive
ripple effect throughout the life of the child.
Pharmacological Treatment Dilemmas
It is often difficult to obtain accurate
information regarding side effects and treatment response in child patients.
Parents, children and psychiatrists, in spite of a good collaborative effort,
may have different understandings of the target symptoms, side-effect pro-file,
and what constitutes a positive clinical response. This ambi-guity makes any
but the most robust clinical responses difficult to observe. Again, experience
at tertiary referral centers suggests that the lack of a clinical response to
medication in complex pa-tients may often be related to inadequate monitoring
of medicine effects and inadequate treatment trials.
Clinically complex patients may not have a robust
re-sponse to a single medication but may require multiple medica-tion trials to
identify which medications offer the most benefit, and in which combination.
Sequential treatment trials are dif-ficult for all involved, especially
children and families, who are often looking for a single powerful intervention.
With the added complexity of treatment, there is the added risk of confusion
and the need for an excellent psychiatristŌĆōpatientŌĆōfamily relation-ship. In
those cases in which the relationship is not optimal, it is possible that a
patient may not have the maximal clinical benefit of pharmacological
interventions.
With increasing numbers of available psychotropic
medi-cations, psychiatrists become increasingly less experienced with the range
of clinical effects and side effects in individual medica-tions. In clinically
complex patients, the prescription of unfamil-iar medications may be necessary
but may add to the risk that a trial will be discontinued prematurely because
of doubt about a side effect. In addition, unusual side effects, such as the apathy
or disinhibition syndromes seen with some patients receiving the specific
serotonin reuptake inhibitors, may go unnoticed and add to clinical morbidity.
Whereas pharmacological interventions offer great
prom-ise, clinical experience suggests that excellent diagnostic skills, good
relationships with the patient and family, time, and a keen eye for effects and
side effects are necessary for benefits to be realized. Less intensive efforts
may make patients appear more complex than necessary.
Related Topics