Chapter: Essentials of Psychiatry: Childhood Disorders: Tic Disorders
Tic Disorders: Standard Approaches to Treatment
Standard Approaches to Treatment
Educate the Patient and Family
The initiation of treatment can be a delicate
process, given the difficulties patients and their families experience before
finding appropriate care. Most families are frightened about their child’s
having a neuropsychiatric disorder and envision a grim progno-sis. After the
evaluation is completed, often in the first session, general education of the
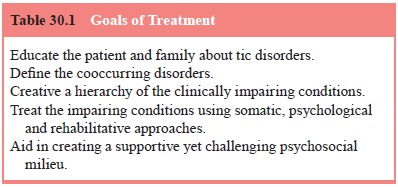
patient and family about the course of the tic disorder is essential (Table
30.1). Most patients and fami-lies are relieved to hear that the majority of
persons with tics have consistent improvement in tic severity as they move
through their teenage years and into adulthood. They are also pleased to hear
that tic symptoms are not inherently impairing.
Identify Cooccurring Disorders
Identifying whether ADHD, LD and OCD are present is
espe-cially important because they are often the more common im-pairing
conditions in these children. One of the major pitfalls of treatment of
patients with Tourette’s disorder is to pursue tic sup-pression to the
exclusion of the treatment of other cooccurring conditions that are present and
possibly more impairing.
Create a Hierarchy of the Clinically Impairing Conditions
Most psychiatrists, as part of their formulation,
create some clini-cal hierarchy; yet in Tourette’s disorder, with the multitude
of often complex problems, it is essential that a conscious effort be made to
formulate, organize and create hierarchies for treatment. For example children
with moderate tics and separation anxiety with school refusal should be
considered for a treatment with selective serotonin reuptake inhibitor (SSRI)
for their separation anxiety rather than neuroleptics for tic suppression (The
Research Unit on Pediatric Psychopharmacology Anxiety Study Group, 2001). It is
possible with successful treatment of the anxiety disorder that patient may
also experience a reduction in tic severity also.
Treat the Impairing Conditions
Tic Suppression: Pharmacological
The goal of pharmacological treatment is the
reduction of tic severity, not necessarily the elimination of tics. Haloperidol
has been used effectively to suppress motor and phonic tics for more than 30
years. Since that time, a number of other neuroleptic agents have also been
identified as useful in tic suppression, in-cluding fluphenazine and pimozide.
In Europe, the substituted benzamides, sulpiride and tiapride, and the
nonneuroleptic tetrabenazine have also been shown to be useful. As new
neu-roleptic agents become available, clinical trials for tic suppres-sion
invariably occur. Preliminary results with risperidone have been mixed, whereas
trials with clozapine are more uniformly negative. The major drawback with
neuroleptic agents is the fre-quent and significant side effects, which often
preclude continued use of the medication.
Haloperidol
Haloperidol is a high-potency neuroleptic that
preferentially blocks dopamine D2 receptors. Historically,
haloperidol has been the most frequently used medication for tic suppression.
It is ef-fective in a clear majority of patients, although relatively few
pa-tients are willing to tolerate the side effects to obtain the
tic-sup-pressing benefits. Neuroleptics are often effective at low doses, and
low doses minimize side effects. For haloperidol, doses in the range of 0.5 to
2.0 mg/day are usually adequate. Starting dosages are low (0.25–0.5 mg/day),
with small increases in dose (0.25–0.5 mg/day) every 5 to 7 days. Most often
the medication is given at bedtime, but with low doses, some patients may
require twice-a-day dosing for good tic control.
Side effects with all neuroleptics are common and
include sedation, acute dystonic reactions, extrapyramidal symptoms including
akathisia, weight gain, cognitive dulling and the com-mon anticholinergic side
effects. There have also been reports of subtle, difficult to recognize side
effects with neuroleptics, in-cluding clinical depression, separation anxiety,
panic attacks and school avoidance.
Dosage reduction is the most prudent response to
side ef-fects, although the addition of medications such as benztropine for the
extrapyramidal symptoms can be useful. Dosage reduc-tion in those children with
Tourette’s disorder who have been administered neuroleptics long term may be
complicated by withdrawal dyskinesias and significant tic worsening or rebound.
Withdrawal dyskinesias are choreoathetoid movements of the orofacial region,
trunk and extremities that appear after neu-roleptic discontinuation or dosage
reduction and tend to resolve in 1 to 3 months. Tic worsening even above
pretreatment baseline level (i.e., rebound) can last up to 1 to 3 months after
discontinu-ation or dosage reduction. Tardive dyskinesia, which is similar in
character to withdrawal dyskinesia, most often develops during the course of
treatment or is “unmasked” with dosage reductions. Rarely have cases of tardive
dyskinesia been reported to occur in patients with Tourette’s disorder.
Fluphenazine
Whereas fluphenazine has never undergone controlled
trials, clinical experience suggests that it has somewhat fewer side effects
than haloperidol. Fluphenazine has both dopamine D1 and D2
receptor-blocking activity, and the side effect profile is similar to that of
haloperidol. Fluphenazine is slightly less potent than haloperidol so that
starting doses are somewhat higher (0.5–1 mg/day), as are treatment doses (3–5
mg/day).
Pimozide
Pimozide is a potent and specific blocker of
dopamine D2 recep-tors. Its side-effect profile is generally similar
to that of the other neuroleptics, although it has fewer sedative and
extrapyramidal side effects than haloperidol. In contrast to either haloperidol
or fluphenazine, pimozide has calcium channel blocking properties that affect
cardiac conduction, as evidenced by changes in the electrocardiogram. The
coadministration of other medications that affect cardiac conduction, such as
the tricyclic antidepres-sants (TCAs), is generally contraindicated. Baseline
and follow-up electrocardiograms are important for adequate management of
patients.
Beginning treatment with a dose of 1 mg/day is
prudent, although with pimozide’s long half-life, every-other-day dos-ing can
be used to decrease the effective daily dose. Increases of up to 1 mg/day can
occur every 5 to 7 days until symptoms are controlled. Most patients experience
clinical benefit with few side effects with doses of 1 to 4 mg/day. Higher doses
can be associated with more side effects. In a comparison of pimozide,
haloperidol and no drug in patients with Tourette’s disorder and ADHD, pimozide
at 1 to 4 mg/day was useful in decreasing tics and improving some aspects of
cognition that are commonly im-paired in ADHD (Sallee and Rock 1994). The
potential to have impact on both Tourette’s disorder and ADHD symptoms with a
single drug is a clear advantage that pimozide may have over other
neuroleptics.
Atypical Neuroleptics
The atypical neuroleptics appear to have replaced
the standard neuroleptics as the mainstay of treatment for the psychotic
dis-orders. Given the potentially lower risk for tardive dyskinesia with these
agents, their efficacy has been assessed for tic sup-pression in patients with Tourette’s
disorder. To date there are only small controlled or open trials to guide the
clinician in the use of these agents. Clozapine does not appear to be effective
as a tic-suppressing agent and its hematological side effects preclude its use.
Risperidone has been effective in reducing tic symptoms severity in one
controlled trial (Dion et al., 2002)
and may have the added benefit of augmenting SSRIs in treating tic-related OCD.
Olanzapine in low doses does not appear to have the
same tic-suppressing power as the typical neuroleptics which may be related to
olanzapine’s relatively weak dopamine D2 blocking activity. Side
effects, especially weight gain, have dampened the enthusiasm for the atypicals
risperidone, olanzapine and quetiapine. In one of the larger placebo-controlled
trials (N 5 56) of
the new neuroleptics, ziprasidone was found to be effective in reducing tic
symptoms. The mean dose was low 28 ± 10
mg/day. There were few side effects including a low incidence of weight gain
(Gilbert et al., 2000).
Clonidine and Guanfacine
Whereas controlled trials have shown that some
patients ben-efit with symptom reduction, the overall effect of clonidine for
tic suppression and ADHD is more modest than that achieved with the “gold
standards” (haloperidol and the stimulants, re-spectively) for these conditions
(Goetz, 1993). Given clonidine’s mild side-effect profile, it is often the
first drug used for tic suppression, especially in those children with
Tourette’s disor-der and ADHD. Treatment is initiated at 0.025 mg/day and
in-creased in increments of 0.025 to 0.05 mg/day every 3 to 5 days or as side
effects (sedation) allow. Usual effective treatment doses are in the range of
0.1 to 0.3 mg/day and are given in di-vided doses (4–6 hours apart). Higher doses
are associated with side effects, primarily sedation, and are not necessarily
more effective. The onset of action is slower for tic suppression (3–6 weeks)
than for ADHD symptoms. Side effects, in addition tosedation, include
irritability, headaches, decreased salivation, and hypotension and dizziness at
higher doses. Interestingly, owing to clonidine’s short half-life, some
patients experience mild withdrawal symptoms between doses. More severe
re-bound in autonomic activity and tics can occur if the medica-tion is
discontinued abruptly. Some patients find that clonidine in the transdermal
patch form provides a more stable clinical effect and avoids multiple doses
each day. Children are usually stabilized on oral doses before they are
switched to the patch. A rash at the site of the patch is a common, but
manageable, complication of treatment.
Guanfacine is an alpha-2-adrenergic agonist that
poten-tially offers greater benefit than clonidine because of differ-ences in
site of action, side effects and duration of action. In nonhuman primates,
guanfacine appears to bind preferentially with alpha-2-adrenergic receptors in
prefrontal cortical re-gions associated with attentional and organizational
functions. Guanfacine’s long half-life offers the advantage of twice-a-day
dosing, which is more convenient than the multiple dosing required with
clonidine. In a randomized, placebo-controlled trial (N 5 31) of children with tics and ADHD, guanfacine in
doses up to 0.3 mg/day had an average 31% reduction in tic severity compared
with no reduction on placebo. Clinically the effect on tics is less than would
be expected on neuroleptics (Scahill et
al., 2001).
Benzodiazepines
Benzodiazepines can be useful in decreasing
comorbid anxiety in patients with Tourette’s disorder. In addition, clonazepam
ap-pears also to be useful in selected patients for tic reduction. Of-ten,
doses of 3 to 6 mg/day may be necessary for tic reduction. Because sedation is
a significant side effect at these dosages, an extended titration phase of 3 to
6 months may be necessary. Simi-larly, a slow taper is required to avoid
withdrawal symptoms.
Pergolide
Agonist activity on presynaptic dopamine neurons
results in decrease dopamine release and may therefore result in decreased tic
severity in people with Tourette’s disorder. To exploit this finding a number
of small open trials of dopamine agonists and a small controlled trial of
pergolide (N 5 24) have
been conducted. Pergolide, a mixed D1–D2–D3
dopamine agonist often used for restless leg syndrome, was found to be superior
to placebo in reducing tic severity and was associated with few adverse events
(Gilbert et al., 2000). Doses used
were low as higher doses may be associated with dopamine agonist effects
postsynaptically.
Baclofen
Baclofen, a muscle relaxant, is GABA-B receptor
agonist that acts presynaptically to inhibit the release of excitatory amino
acids such as glutamate. In a small placebo controlled crossover trial (N 5 10) baclofen 20 mg t.i.d. was
not found to be effective in reducing tic severity but did appear to have an
effect on tic-related impairment (Singer et
al., 2001).
Infection and Autoimmune-based Treatments
Several treatment studies have been undertaken
based on the hy-pothesis that some forms of Tourette’s disorder or OCD may be
related to streptococcal infection. Based on the beneficial effects of
penicillin prophylaxis in preventing recurrences of rheumatic fever, a similar
strategy was employed in subjects meeting cri-teria for PANDAS (Garvey et al., 1999). The study was limited by
a number of flaws and although the concept of prophylaxis is compelling,
special design considerations will be required in future studies.
After small open trials with the immunomodulatory
treat-ments such as plasma exchange or intravenous immunoglobulin (IVIG), a
larger trial comparing these methods to sham IVIG was undertaken. Children
meeting criteria for PANDAS (N 5 30) were
randomly assigned (1 : 1 : 1) to treatment with plasma exchange (five
single-volume exchanges over 2 weeks), IVIG (1 g/kg daily on two consecutive
days), or placebo (saline solution given in the same manner as IVIG) and
subjects were reported as doing well at 1 year (Lougee et al., 2000). Although this study is encour-aging there are a
number of methodological problems including lack of a placebo control for
plasma exchange and inclusion of uncontrolled subjects in outcome analysis
after the first month. These findings do support ongoing investigation of these
treat-ment methods but given the cost, risk and highly experimental nature of
these treatments it is recommended that patients obtain these treatments only
in the context of ongoing clinical inves-tigations of these treatments at major
medical research centers (for further information, see http://intramural.nimh.nih.gov/re-search/pdn/web.htm).
Tic Suppression: Nonpharmacological
The behavioral technique shown to be most effective
is habit reversal training. For Tourette’s disorder, habit reversal training is
the use of a competing muscle contraction or behavioral re-sponse that opposes
the tic movement. This method is usually combined with relaxation training,
self-monitoring, awareness training and positive reinforcement. In the few
published studies of habit reversal training, there were marked overall
reductions in tic frequency. Treatment averaged 20 training sessions during an
8- to 11-month period. Marked tic reduction was noted at 3 to 4 months.
Interestingly, urges or sensations experienced before the tic movements also
decreased with behavioral treatment (Azrin and Peterson, 1990).
Psychosocial Treatments
There are no published systematic studies of
psychosocial in-terventions for patients with Tourette’s disorder. Most
treatment efforts are based on a combination of traditional psychosocial in-terventions
and clinical judgment.
Education
Perhaps the most useful psychosocial and
educational interven-tion is to make the patient aware of the Tourette Syndrome
Asso-ciation, both national and local c-hapters. This and other self-help
groups can be useful as a source of support and education for patients,
families and psychiatrists.
Therapy
Individual psychotherapy can be useful for support,
develop-ment of awareness, or addressing personal and interpersonal problems
more effectively. Family therapy can be useful when families have problems
adjusting, functioning and communicat-ing. Although most families do well, some
families have difficul-ties understanding the involuntary nature of tics and
may punish their children for their tics, even after diagnosis and education.
Alternatively, some families have more behavior difficulties with their
children after diagnosis than before. Many parents of chil-dren with Tourette’s
disorder inadvertently lower general behav-ior expectations because of confusion
about what behaviors areand are not tics, or because of the parents’ desire not
to add any additional stress to the youngster’s life. Also, with confusion in
the field regarding the scope of problems in Tourette’s disorder, some parents
see all maladaptive behaviors as involuntary and do not hold their children
responsible for their behaviors. For chil-dren with Tourette’s disorder to do
well, they need support from their family to develop effective self-control in
areas not affected by Tourette’s disorder so that optimal adaptation can occur.
In newly diagnosed adults, psychotherapy oriented
toward adequate adjustment to the diagnosis is important but not always easy.
Adult patients frequently experience a mixture of relief to be finally
diagnosed, with anger and resentment related to their past experiences with
discrimination or inadequate medical care. Severely affected adults may also
need psychotherapy to deal with the psychological and psychosocial difficulties
related to having a chronic illness.
Other Psychosocial Interventions
For children, active intervention at school is
essential to create a supportive yet challenging academic and social
environment. Ef-forts to educate teachers, principals and other students can
result in increased awareness of Tourette’s disorder and tolerance for the
child’s symptoms.
Many young adults are finding Tourette’s disorder
support and social groups important for interpersonal contact and con-tinued
adult development. Efforts to keep people with Tourette’s disorder working are
important, as are rehabilitation efforts for those who are not working. Finding
housing and obtaining disa-bility or public assistance may be necessary for the
most disabled patients with Tourette’s disorder.
Genetic Counseling
One question commonly asked by young adults with
Tourette’s disorder is their risk for having a child with Tourette’s disorder.
Given the fact that many who present for clinical attention with Tourette’s
disorder have comorbid conditions, genetic counseling of people with Tourette’s
syndrome should include not only the risk for Tourette’s disorder but also the
risk for other neuropsy-chiatric problems such as ADHD or OCD that may be part
of the young person’s history. In addition, because the base rate of
neu-ropsychiatric disorders is high, it is not uncommon for spouses of people
with Tourette’s disorder to have a neuropsychiatric disorder. In providing
counseling to these couples it is impor-tant that genetic counseling be
conducted not just about Tourette syndrome, but about the other conditions that
occur as part of the young couple’s history.
Related Topics