Chapter: Obstetric and Gynecological Nursing : Abnormal Labour
Post partum Hemorrhage
Post partum Hemorrhage
Definition:-Post partum hemorrhage is
bleeding from thegenital tract during the 3rd stage of labour, or with in 24 hours after
delivery of the placenta to the amount of 500ml or any amount that will change
the patient’s condition
It is responsible for maternal deaths and is one of the emergencies in
which if the Nurse/ mid wife does not know how or fails to play the part the
doctor may be Unable to save the mother’s life as shock gets in quickly and can
become irreversible.
The rate of flow that is more important than the amount Anaemia is a
predisposing cause.
It is occurs within 24 hours at delivery it is caused primary while
after 24 hrs of Delivery is secondary PPH.
Cause of Primary PPH
·
Retained Placenta
·
Retained Cotyledon
·
Genital trauma
·
Disseminated intramuscular coagulation (DIC)
·
Inversion of uterus
Cause of secondary PPH
·
Chorioamnioitis
·
Retained products
Type of PPH
·
Atonic postpartum hemorrhage
·
Traumatic postpartum hemorrhage
·
Hypofibrinogenaemia
Management of PPH
Three basic principle are applied
·
Call an obstetrician
·
Stop the bleeding
·
Resuscitate the mother
1. Atonic Postpartum Hemorrhage (80% of PPH)
This is bleeding from the placental site when the uterus is not well
contracted. This is a failure of a myometrium at the placental site to contract
and retract and to compress torn blood vessels and control blood loss by a
living ligature action.
Cause
·
Incomplete separation of placenta
·
Retained cotyledon, placental fragments or membranes
·
Prolonged labour & obstructed labour resulting in uterine inertia
·
Rapid expulsion of large body
·
Poly hydraminous, multiple pregnancy-over stretnig of the uterus
·
Anteportum hemorrhage
·
Adherent placenta that has partially separated
·
Precipitate labour
·
Full bladder
·
Mismanagement of the ill state of labour
·
Prolonged anesthesia
·
Fibroids
·
Grand mult
Management of atonic PPH
·
Massage uterus
·
Give pitocin or ergometrine
·
Baby to breast
·
Empty bladder
·
Empty uterus
·
Bimanual compression
Bimanual Compression
It can be done externally or internally
Method
Place one hand on the fundus and the other above the Symphsis pubis
(external) or in anterior fornix (internally) and squeeze until clotting occurs
usually clotting takes place 7-10 minutes later. Remove the external hand to
check whether the bleeding is stopped or not
Dangers: -
Hemorrhage
Shock
Infection
2. Traumatic Post Partum Hemorrhage (20% of PPH)
This is bleeding from a laceration of the cervix, vaginal wall, and
perineum episiotomy or even from ruptured uterus.
Cause
·
Delivery through partially dilated cervix
·
Instrumental delivery-bruised
·
Difficult delivery- Face to pubes, after coming head of breech
Management of traumatic PPH
When bleeding is due to the tear, explore the area for the tear, clamp
the bleeding point and suture. Make sure that the uterus is not ruptured. If
the laceration is sutured and bleeding stop make sure that the uterus is well
contacted.
If bleeding is from bruised cervix place a pack against it for a few
minutes to an hour, if so leave catheter in situ.
If bleeding is from ruptured uterus, transfer to the hospital as soon as
possible; go with patient or send a full written report with date, time of
departure and Signature.
3. Hypo Fibrinogenaemia
This is bleeding due to a clothing defect and the patient continuous to
bleeding in spite of treatment for the other types of postpartum hemorrhage.
Causes
·
Placental abraption
·
Intrauterine death which is prolonged
·
Amniotic fluid embolism
·
Pre- eclampsia, eclampsia
·
Intra uterine infection
·
Hepatitis
Management of hypofibrinogenaemia (DIC)
The best treatment is
·
Fresh blood transfusion
·
Fibrinogen or triple strength plasma transfusion
·
Give oxygen and resuscitate with IV dirp
· Drugs as prescribed
·
IV syntocinic if uterus is lax
The patient will respond quickly to this treatment if given quickly.
Advice Hospital delivery for the next time and warm her to explain to doctor or
nurse.
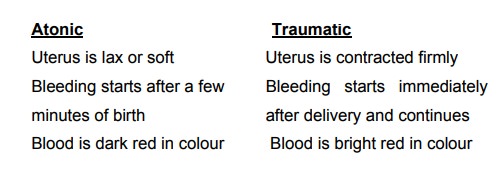
It is important to be able to differentiate between a tonic and
traumatic psot part hemorrhage.
Management of Severe PPH in a Health Center
·
Massage the uterus to stimulate contraction and expel the placenta if
possible
·
Stay with your patient and shout for help
·
Give ergometrine 0.5 ml I.V and put up a drip
·
Empty bladder
·
If placenta is already expelled, expel clots if not try to expel it with
the contraction caused by ergometrine. If not and she is still bleeding
severely in order to save the patient’s life manual removal is done.
· If still the uterus is lax as a last reason, bimanual compression method is done.
Consequences of PPH
·
Shock and collapse- death
·
Puerperal anemia – weakness & low resistance to infection
·
Fear of the further pregnancy
·
Sheehan’s syndrome- due to anterior pituitary necrosis
·
Infection
Prevention of PPH
Good antenatal care
·
Careful history taking to find out if she had PPH in previous delivery.
·
Bring hemoglobin as high as possible and treat anemia. Book high risk
for hospital delivery. Group & cross match high-risk mother in labour
·
Try to prevent prolonged or obstructed labour
·
Make sure that the mother rests as much as possible during 1st stage and prevent dehydration.
·
Keep bladder empty
·
Delivery head slowly and control it
·
Active management of third stage
Related Topics