Chapter: Medical Surgical Nursing: Principles and Practices of Rehabilitation
Nursing Process: The Patient With Impaired Skin Integrity
NURSING PROCESS: THE PATIENT WITH IMPAIRED SKIN
INTEGRITY
An estimated 1.5 to 3 million patients develop pressure ulcers an-nually
(Mayo Clinic Rochester, 2001). Both prevention and treat-ment of pressure
ulcers are costly in terms of health care dollars and quality of life for
patients at risk. Because the cost in terms of pain and suffering for a person
with a pressure ulcer cannot be quanti-fied, all possible efforts should be
made to prevent skin breakdown.
Patients confined to bed for long periods, patients with motor or
sensory dysfunction, and patients who experience muscular at-rophy and
reduction of padding between the overlying skin and the underlying bone are
prone to pressure ulcers. Pressure ulcers are localized areas of infarcted soft
tissue that occur when pressure applied to the skin over time is greater than
normal capillary clo-sure pressure, which is about 32 mm Hg. Critically ill
patients have a lower capillary closure pressure and are at greater risk for
pressure ulcers. The initial sign of pressure is erythema (redness of the skin)
caused by reactive hyperemia, which normally resolves in less than 1 hour.
Unrelieved pressure results in tissue ischemia or anoxia. The cutaneous tissues
become broken or destroyed, leading to progressive destruction and necrosis of
underlying soft tissue, and the resulting pressure ulcer is painful and slow to
heal.
Assessment
Immobility, impaired sensory perception or
cognition, decreased tissue perfusion, decreased nutritional status, friction
and shear forces, increased moisture, and age-related skin changes all
con-tribute to the development of pressure ulcers.
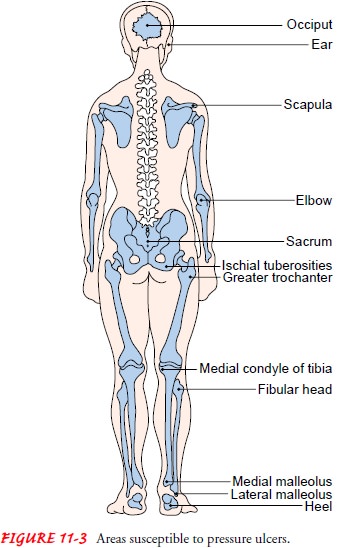
IMMOBILITY
When a person is immobile and inactive, pressure is
exerted on the skin and subcutaneous tissue by objects on which the person
rests, such as a mattress, chair seat, or cast. The development of pressure
ulcers is directly related to the duration of immobility: if pressure continues
long enough, small vessel thrombosis and tis-sue necrosis occur, and a pressure
ulcer results. Weight-bearing bony prominences are most susceptible to pressure
ulcer devel-opment because they are covered only by skin and small amounts of
subcutaneous tissue. Susceptible areas include the sacrum and coccygeal areas,
ischial tuberosities (especially in people who sit for prolonged periods),
greater trochanter, heel, knee, malleolus, medial condyle of the tibia, fibular
head, scapula, and elbow (Fig. 11-3).
IMPAIRED SENSORY PERCEPTION OR COGNITION
Patients with sensory loss, impaired level of consciousness, or
paralysis may not be aware of the discomfort associated with pro-longed
pressure on the skin and, therefore, may not change their position themselves
to relieve the pressure. This prolonged pres-sure impedes blood flow, reducing
nourishment of the skin and underlying tissues. A pressure ulcer may develop in
a short period.
DECREASED TISSUE PERFUSION
Any condition that
reduces the circulation and nourishment of the skin and subcutaneous tissue
(altered peripheral tissue perfu-sion) increases the risk of pressure ulcer
development. Patients with diabetes mellitus experience an alteration in
microcircula-tion. Similarly, patients with edema have impaired circulation and
poor nourishment of the skin tissue. Obese patients have large amounts of
poorly vascularized adipose tissue, which is sus-ceptible to breakdown.
DECREASED NUTRITIONAL STATUS
Nutritional
deficiencies, anemias, and metabolic disorders also contribute to pressure
ulcer development. Anemia, regardless of its cause, decreases the blood’s
oxygen-carrying ability and pre-disposes a patient to pressure ulcer formation.
Patients who have low protein levels or who are in a negative nitrogen balance
ex-perience tissue wasting and inhibited tissue repair. Serum albu-min is a
sensitive indicator of protein deficiency; serum albumin levels of less than 3
g/mL are associated with hypoalbuminemic tissue edema and increased risk of
pressure ulcers. Specific nutri-ents, such as vitamin C and trace minerals, are
needed for tissue maintenance and repair.
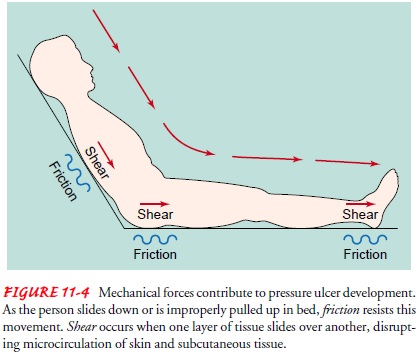
FRICTION AND SHEAR
Mechanical forces also contribute to the development of pres-sure
ulcers. Friction is the resistance to movement that occurs when two surfaces
are moved across each other. Shear is created by the interplay of gravitational
forces (forces that push the body down) and friction. When shear occurs, tissue
layers slide over one another, blood vessels stretch and twist, and the
microcir-culation of the skin and subcutaneous tissue is disrupted. Evi-dence
of deep tissue damage may be slow to develop and maypresent through the
development of a draining tract. The sacrum and heels are most susceptible to
the effects of shear. Pressure ul-cers from friction and shear occur when the
patient slides down in bed (Fig. 11-4) or when the patient is moved or
positioned improperly (eg, dragged up in bed). Spastic muscles and paraly-sis
increase the patient’s vulnerability to pressure ulcers related to friction and
shear.
INCREASED MOISTURE
Prolonged contact with moisture from perspiration, urine, feces, or
drainage produces maceration (softening) of the skin. The skin reacts to the
caustic substances in the excreta or drainage and be-comes irritated. Moist,
irritated skin is more vulnerable to pres-sure breakdown. Once the skin breaks,
the area is invaded by microorganisms (eg, streptococci, staphylococci, Pseudomonasaeruginosa, Escherichia coli),
and infection occurs. Foul-smellinginfectious drainage is present. The lesion
may enlarge and allow a continuous loss of serum, which may further deplete the
body of essential protein needed for tissue repair and maintenance. The lesion
may continue to enlarge and extend deep into the fascia, muscle, and bone, with
multiple sinus tracts radiating from the pressure ulcer. With extensive
pressure ulcers, systemic infections may develop, frequently from gram-negative
organisms.
Gerontologic Considerations
In older adults, the
skin has diminished epidermal thickness, der-mal collagen, and tissue
elasticity. The skin is drier as a result of diminished sebaceous and sweat
gland activity. Cardiovascular changes result in decreased tissue perfusion.
Muscles atrophy, and bone structures become prominent. Diminished sensory
percep-tion and reduced ability to reposition oneself contribute to pro-longed
pressure on the skin. Therefore, the older adult is more susceptible to
pressure ulcers, which cause pain and suffering and reduce quality of life
(Agency for Health Care Policy and Research [AHCPR], 1994).
ADDITIONAL RISK FACTORS
In assessing the patient for potential risk for pressure ulcer devel-opment, the nurse assesses the patient’s mobility, sensory per-ception, cognitive abilities, tissue perfusion, nutritional status, friction and shear forces, sources of moisture on the skin, and age. The nurse
•
Assesses total skin condition at least twice a day
•
Inspects each pressure site for erythema
•
Assesses areas of erythema for blanching response
•
Palpates the skin for increased warmth
•
Inspects for dry skin, moist skin, breaks in skin
•
Notes drainage and odor
•
Evaluates level of mobility
•
Notes restrictive devices (eg, restraints, splints)
•
Evaluates circulatory status (eg, peripheral
pulses, edema)
•
Assesses neurovascular status
•
Determines presence of incontinence
•
Evaluates nutritional and hydration status
•
Reviews the patient’s record for laboratory
studies, includ-ing hematocrit, hemoglobin, electrolytes, albumin,
trans-ferrin, and creatinine
•
Notes present health problems
•
Reviews current medications
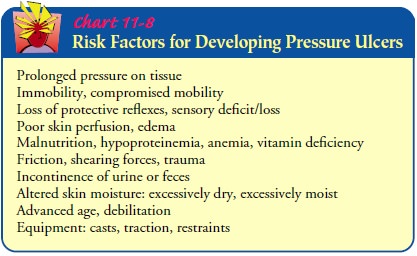
Scales such as the
Braden or Norton scale may be used to fa-cilitate systematic assessment and
quantification of a patient’s risk for pressure ulcer, although the nurse needs
to recognize that the reliability of these scales is not well established. They
tend to over-estimate those at risk and may promote unwarranted use of costly
preventive equipment. See Chart 11-8 for a list of risk factors for development
of pressure ulcers.
If a pressure area is noted, the nurse notes its size and location and
may use a grading system to describe its severity (see Chart 11-9). Generally,
a stage I pressure ulcer is an area of nonblanch-able erythema, tissue
swelling, and congestion, and the patient complains of discomfort. The skin
temperature is elevated be-cause of the increased vasodilation. The redness
progresses to a dusky, cyanotic blue-gray appearance, which is the result of
skin capillary occlusion and subcutaneous weakening.
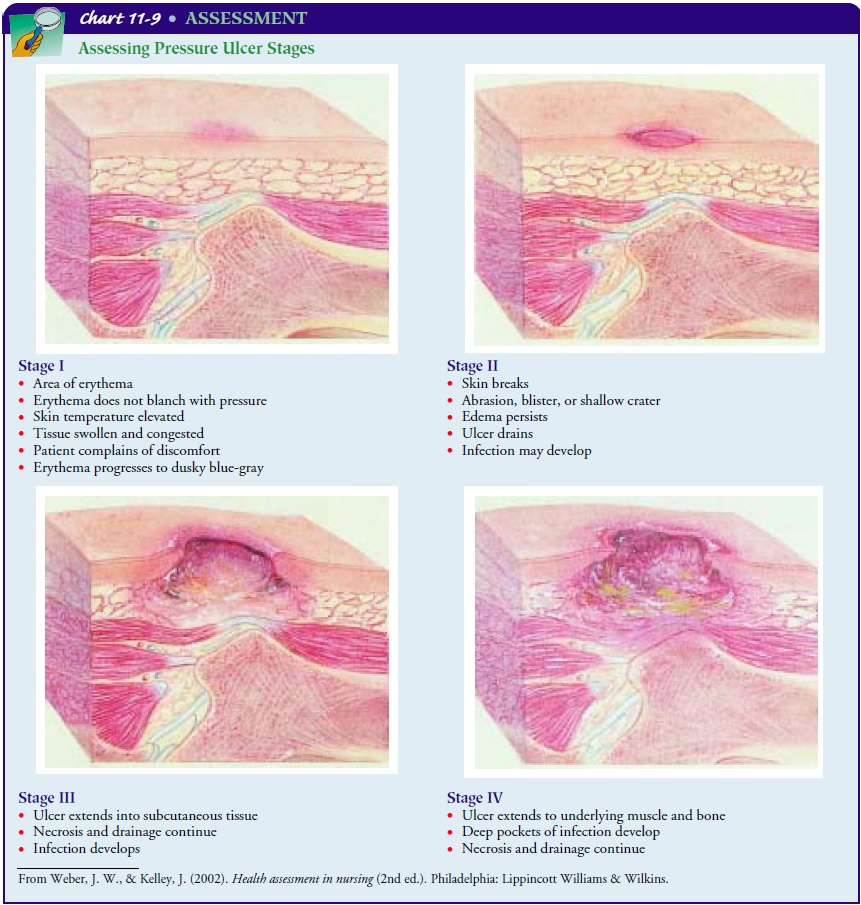
A stage II pressure ulcer exhibits a break in the skin through the
epidermis or the dermis. An abrasion, blister, or shallow crater may be seen.
Necrosis occurs along with venous sludging and throm-bosis and edema with
cellular extravasation and infiltration.
A stage III pressure ulcer extends into the subcutaneous tissues.
Clinically, a deep crater with or without undermining of adjacent tissues is
noted.
A stage IV pressure ulcer extends into the
underlying structures, including the muscle and, possibly, the bone. The skin
lesion may appear insignificant when in reality, beneath the small surface
ulcer is a large undermined area of necrotic tissue.
The appearance of
purulent drainage or foul odor suggests an infection. With an extensive
pressure ulcer, deep pockets of infec-tion are often present. Drying and
crusting of exudate may be present. Infection of a pressure ulcer may advance
to osteomyelitis, pyarthrosis (pus formation within a joint cavity), sepsis,
and septic shock.
Nursing Diagnosis
Based on the assessment
data, the nursing diagnoses may include the following:
· Risk for impaired skin
integrity
· Impaired skin integrity
(related to immobility, decreased sensory perception, decreased tissue
perfusion, decreased nutritional status, friction and shear forces, increased
mois-ture, or advanced age)
Planning and Goals
The major goals for the
patient may include relief of pressure, improved mobility, improved sensory
perception, improved tis-sue perfusion, improved nutritional status, minimized
friction and shear forces, dry surfaces in contact with skin, and healing of
pressure ulcer, if present.
Nursing Interventions
RELIEVING PRESSURE
Frequent changes of position are needed to relieve and redistrib-ute the
pressure on the patient’s skin and to prevent prolonged reduced blood flow to
the skin and subcutaneous tissues. This can be accomplished by teaching the
patient to change position or by turning and repositioning the patient. The patient’s
family mem-bers should be taught how to position and turn the patient at home
to prevent pressure ulcers. Shifting weight allows the blood to flow into the
ischemic areas and helps the tissues recover from the effects of pressure.
Thus, the patient should be cared for as follows:
•
Turned and repositioned at 1-hour to 2-hour
intervals
•
Encouraged to shift weight actively every 15
minutes
POSITIONING THE PATIENT
The patient should be
positioned laterally, prone, and dorsally in sequence unless a position is not
tolerated or is contraindicated. The recumbent position is preferred to the
semi-Fowler’s posi-tion because of increased supporting body surface area in
this po-sition. In addition to regular turning, there should be small shifts of
body weight, such as repositioning of an ankle, elbow, or shoulder. The skin is
inspected at each position change and as-sessed for temperature elevation. If
redness or heat is noted or if the patient complains of discomfort, pressure on
the area must be relieved.
Another way to relieve
pressure over bony prominences is the bridging technique, accomplished through
the correct position-ing of pillows. Just as a bridge is supported on pillars
to allow traf-fic to move underneath, so can the body be supported by pillows
to allow for space between bony prominences and the mattress. A pillow or
commercial heel protector may be used to support the heels off the bed when the
patient is supine. Placing pillows su-perior and inferior to the sacrum
relieves sacral pressure. Sup-porting the patient in a 30-degree side-lying
position avoids pressure on the trochanter. In the aging patient, frequent
small shifts of body weight may be effective. Placing a small rolled towel or
sheepskin under a shoulder or hip will allow a return of blood flow to the skin
in the area on which the patient is sitting or lying. The towel or sheepskin is
moved around the patient’s pressure points in a clockwise fashion.
USING PRESSURE-RELIEVING DEVICES
At times, special
equipment and beds may be needed to help re-lieve the pressure on the skin.
These are designed to provide sup-port for specific body areas or to distribute
pressure evenly.
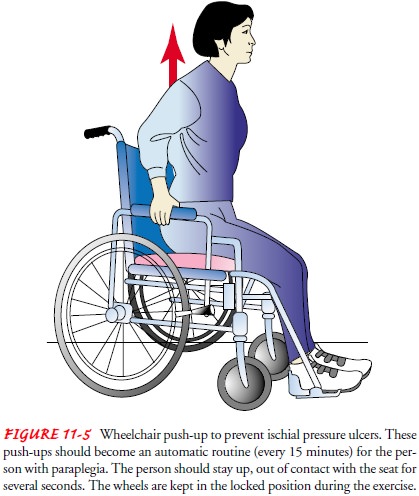
Patients sitting in wheelchairs for prolonged periods should have
wheelchair cushions fitted and adjusted on an individualized basis, using
pressure measurement techniques as a guide to selec-tion and fitting. The aim
is to redistribute pressure away from areas at risk for ulcers, but no cushion
is able to eliminate exces-sive pressure completely. The patient should be
reminded to shift weight frequently and to rise for a few seconds every 15
minutes while sitting in a chair (Fig. 11-5).
Static support devices (such as high-density foam, air, or liq-uid mattress overlays) distribute pressure evenly by bringing more of the patient’s body surface into contact with the supporting sur-face. Gel-type flotation pads and air-fluidized beds reduce pres-sure. The weight of a body floating on a fluid system is evenly distributed over the entire supporting surface (according to Pas-cal’s law). Therefore, as the patient’s body sinks into the fluid, additional surface becomes available for weight bearing, body weight per unit area is decreased, and there is less pressure on the body parts.
Soft, moisture-absorbing padding is also useful because the softness and
resilience of padding provides for more even distrib-ution of pressure and the
dissipation and absorption of moisture, along with freedom from wrinkles and
friction. Bony promi-nences may be protected by gel pads, sheepskin padding, or
soft foam rubber beneath the sacrum, the trochanters, heels, elbows, scapulae,
and back of the head when there is pressure on the sites.
Specialized beds have been designed to prevent pressure on the skin.
Air-fluidized beds float the patient. Dynamic support sur-faces, such as low
air-loss pockets, alternately inflate and deflate sections to change support
pressure for very high-risk patients who are critically ill and debilitated and
cannot be repositioned to relieve pressure. Oscillating or kinetic beds change
pressure by means of rocking movements of the bed that redistribute the
pa-tient’s weight and stimulate circulation. These beds are frequently used
with patients who have injuries due to multiple trauma.
IMPROVING MOBILITY
The patient is
encouraged to remain active and is ambulated whenever possible. When sitting,
the patient is reminded to change positions frequently to redistribute weight.
Active and passive exercises increase muscular, skin, and vascular tone. Ac-tivity
stimulates circulation, which relieves tissue ischemia, the forerunner of
pressure ulcers. For the patient at risk for pressure ulcers, turning and
exercise schedules are essential: repositioning must occur around the clock.
IMPROVING SENSORY PERCEPTION
The nurse helps the
patient recognize and compensate for altered sensory perception. Depending on
the origin of the alteration (eg, decreased level of consciousness, spinal cord
lesion), specific interventions are selected. Strategies to improve cognition
and sensory perception may include stimulating the patient to in-crease
awareness of self in the environment, encouraging the pa-tient to participate
in self-care, or supporting the patient’s efforts toward active compensation
for loss of sensation (eg, a paraplegic patient lifting up from the sitting
position every 15 minutes). When decreased sensory perception exists, the
patient and care-giver are taught to inspect potential pressure areas visually
every morning and evening, using a mirror if necessary, for evidence of
pressure ulcer development.
IMPROVING TISSUE PERFUSION
Exercise and
repositioning improve tissue perfusion. Massage of erythematous areas is
avoided because damage to the capillaries and deep tissue may occur.
In patients who have evidence of compromised peripheral cir-culation
(eg, edema), positioning and elevation of the edematous body part to promote
venous return and diminish congestion im-prove tissue perfusion. In addition,
the nurse or family must be alert to environmental factors (eg, wrinkles in
sheets, pressure of tubes) that may contribute to pressure on the skin and
dimin-ished circulation and remove the source of pressure.
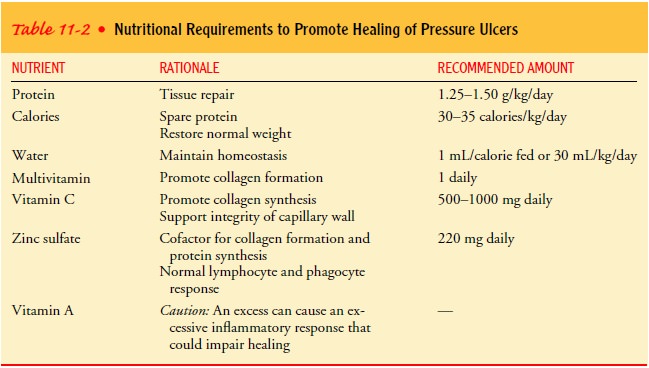
IMPROVING NUTRITIONAL STATUS
The patient’s nutritional status must be adequate, and a positive nitrogen
balance must be maintained, because pressure ulcers de-velop more quickly and
are more resistant to treatment in patients with nutritional disorders. A
high-protein diet with protein sup-plements may be helpful. Iron preparations
may be necessary to raise the hemoglobin concentration so that tissue oxygen
levels can be maintained within acceptable limits. Ascorbic acid (vitamin C) is
necessary for tissue healing. Other nutrients associated with healthy skin
include vitamin A, B vitamins, zinc, and sulfur. With balanced nutrition and
hydration, the skin is able to remain healthy, and damaged tissues can be
repaired (Table 11-2).To assess nutritional status response to therapeutic
strategies, the nurse monitors the patient’s hemoglobin, albumin, and body
weight weekly.
REDUCING FRICTION AND SHEAR
Shear occurs when the
patient is pulled, is allowed to slump, or moves by digging heels or elbows
into the mattress. Raising the head of the bed by even a few centimeters
increases the shearing force over the sacral area; therefore, the semireclining
position is avoided in patients at risk. Proper positioning with adequate
sup-port is also important when a patient is sitting in a chair. Poly-ester
sheepskin pads are thought to reduce shear and friction and may be used with
at-risk patients.
MINIMIZING IRRITATING MOISTURE
Continuous moisture on the skin must be prevented by meticu-lous
hygienic measures. Perspiration, urine, stool, and drainage must be removed
from the skin promptly. The soiled skin should be washed immediately with mild
soap and water and blotted dry with a soft towel. The skin may be lubricated
with a bland lotion to keep it soft and pliable. Drying agents and powders are
avoided. Topical barrier ointments (eg, petroleum jelly) may be helpful in
protecting the skin of patients who are incontinent.
Absorbent pads that wick
moisture away from the body should be used to absorb drainage. Patients who are
incontinent need to be checked regularly
and have their wet incontinence pads and linens changed promptly. Their skin
needs to be cleansed and dried promptly.
PROMOTING PRESSURE ULCER HEALING
Regardless of the stage of the pressure ulcer, the pressure on the area must be eliminated, because the ulcer will not heal until all pressure is removed. The patient must not lie or sit on the pressure ulcer, even for a few minutes. Individualized positioning and turning schedules must be written in the plan of nursing care and followed meticulously.
In addition, inadequate
nutritional status and fluid and elec-trolyte abnormalities must be corrected
to promote healing. Wounds that drain body fluids and protein place the patient
in a catabolic state and predispose to hypoproteinemia and serious secondary
infections. Protein deficiency must be corrected to heal the pressure ulcer.
Carbohydrates are necessary to “spare” the protein and to provide an energy
source. Vitamin C and trace el-ements, especially zinc, are necessary for
collagen formation and wound healing.
Stage I Pressure Ulcers
To permit healing of
stage I pressure ulcers, the pressure is re-moved to allow increased tissue
perfusion, nutritional and fluid and electrolyte balance are maintained,
friction and shear are re-duced, and moisture to the skin is avoided.
Stage II Pressure Ulcers
Stage II pressure ulcers have broken skin. In addition to measures
listed for stage I pressure ulcers, a moist environment, in which migration of
epidermal cells over the ulcer surface occurs more rapidly, should be provided
to aid wound healing. The ulcer is gently cleansed with sterile saline
solution. Use of a heat lamp to dry the open wound is avoided, as is use of
antiseptic solutions that damage healthy tissues and delay wound healing.
Semipermeable occlusive dressing, hydrocolloid wafers, or wet saline dressings
are helpful in providing a moist environment for healing and in min-imizing the
loss of fluids and proteins from the body.
Stage III and IV Pressure Ulcers
Stage III and IV pressure ulcers are characterized by extensive tissue
damage. In addition to measures listed for stage I, these advanced draining,
necrotic pressure ulcers must be cleaned (débrided) to create an area that will
heal. Necrotic, devitalized tissue favors bacterial growth, delays granulation,
and inhibits healing. Wound cleaning and dressing are uncomfortable;
there-fore, the nurse must prepare the patient for the procedure by ex-plaining
what will occur and administering prescribed analgesia.
Débridement may be accomplished by wet-to-damp dressing changes, mechanical
flushing of necrotic and infective exudate, application of prescribed enzyme
preparations that dissolve necrotic tissue, or surgical dissection. If an
eschar covers the ulcer, it is re-moved surgically to ensure a clean, vitalized
wound. Exudate may be absorbed by dressings or special hydrophilic powders,
beads, or gels. Cultures of infected pressure ulcers are obtained to guide
selection of antibiotic therapy.
After the pressure ulcer
is clean, a topical treatment is pre-scribed to promote granulation. New
granulation tissue must be protected from reinfection, drying, and damage, and
care should be taken to prevent pressure and further trauma to the area.
Dress-ings, solutions, and ointments applied to the ulcer should not dis-rupt
the healing process. Multiple agents and protocols are used to treat pressure
ulcers, but consistency is an important key to success. Objective evaluation of
the pressure ulcer (eg, measure-ment of the pressure ulcer, inspection for
granulation tissue) for response to the treatment protocol must be made every 4
to 6 days. Taking photographs at weekly intervals is a reliable strat-egy for
monitoring the healing process, which may take weeks to months to complete.
Surgical intervention is
necessary when the ulcer is extensive, when potential complications (eg,
fistula) exist, and when the ulcer does not respond to treatment. Surgical
procedures in-clude débridement, incision and drainage, bone resection, and
skin grafting.
PREVENTING RECURRENCE
Recurrence of pressure
ulcers should be anticipated; therefore, ac-tive, preventive intervention and
frequent continuing assessments are essential. The patient’s tolerance for
sitting or lying on the healed pressure area is increased gradually by
increasing the time that pressure is allowed on the area in 5- to 15-minute
incre-ments. The patient is taught to increase mobility and to follow a regimen
of turning, weight shifting, and repositioning. The pa-tient teaching plan
includes instruction on strategies to reduce the risk for development of
pressure ulcers and methods to detect, in-spect, and minimize pressure areas.
Early recognition and inter-vention are keys to long-term management of
potential impaired skin integrity.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient
outcomes may include:
Maintains intact skin
a) Exhibits no areas of
nonblanchable erythema at bony prominences
b) Avoids massage of bony
prominences
c) Exhibits no breaks in
skin
Limits pressure on bony prominences
a) Changes position every 1
to 2 hours
b) Uses bridging techniques
to reduce pressure
c) Uses special equipment
as appropriate
d) Raises self from seat of
wheelchair every 15 minutes
Increases mobility
a) Performs range-of-motion
exercises
b) Adheres to turning
schedule
c) Advances sitting time as
tolerated
Sensory and cognitive ability improved
a) Demonstrates improved
level of consciousness
b) Remembers to inspect
potential pressure ulcer areas every morning and evening
Demonstrates improved tissue perfusion
a) Exercises to increase
circulation
b) Elevates body parts
susceptible to edema
Attains and maintains adequate nutritional status
a) Verbalizes the
importance of protein and vitamin C in diet
b) Eats diet high in
protein and vitamin C
c) Maintains hemoglobin,
electrolyte, albumin, transfer-rin, and creatinine levels at acceptable levels
Avoids friction and shear
a) Avoids semireclining
position
b) Uses sheepskin pad and
heel protectors when appropriate
c) Lifts body instead of
sliding across surfaces
Maintains clean, dry skin
a) Avoids prolonged contact
with wet or soiled surfaces
b) Keeps skin clean and dry
c) Uses lotion to keep skin
lubricated
Experiences healing of pressure ulcer
a) Avoids pressure on area
b) Improves nutritional
status
c) Participates in
therapeutic regimen
d) Demonstrates behaviors
to prevent new pressure ulcers
e) States early indicators
of pressure ulcer development
Related Topics