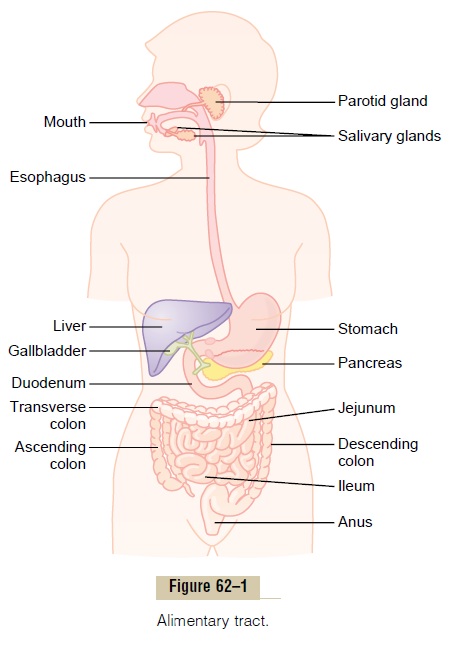
Chapter: Medical Physiology: General Principles of Gastrointestinal Function- Motility, Nervous Control, and Blood Circulation
General Principles of Gastrointestinal Motility
General Principles of Gastrointestinal Motility
Physiologic Anatomy of the Gastrointestinal Wall
Figure 62–2 shows a typical cross section of the intestinal wall, including the fol-lowing layers from outer surface inward: (1) the serosa, (2) alongitudinal musclelayer, (3) a circular muscle layer, (4) the submucosa, and (5) the mucosa. In addi-tion, sparse bundles of smooth muscle fibers, themucosal muscle, lie in the deeper layers of the mucosa. The motor functions of the gut are performed by the different layers of smooth muscle.
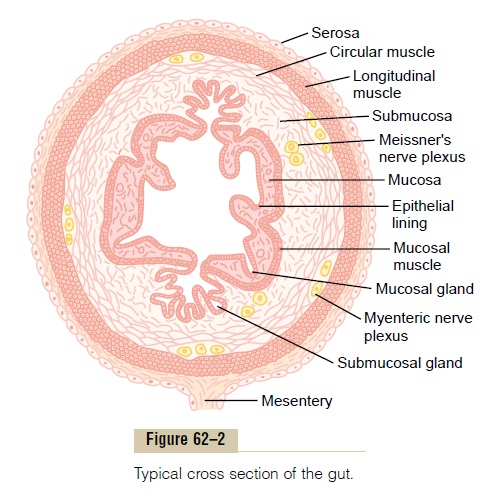
Gastrointestinal Smooth Muscle Functions as a Syncytium. The individual smoothmuscle fibers in the gastrointestinal tract are 200 to 500 micrometers in length and 2 to 10 micrometers in diameter, and they are arranged in bundles of as many as 1000 parallel fibers. In the longitudinal muscle layer, the bundles extend longitudinally down the intestinal tract; in the circular muscle layer, they extend around the gut.
Within each bundle, the muscle fibers are electrically connected with one another through large numbers of gap junctions that allow low-resistance movement of ions from one muscle cell to the next. Therefore, electrical signals that initiate muscle contractions can travel readily from one fiber to the next within each bundle but more rapidly along the length of the bundle than sideways.
Each bundle of smooth muscle fibers is partly separated from the next by loose connective tissue, but the muscle bundles fuse with one another at many points, so that in reality each muscle layer represents a branching latticework of smooth muscle bundles. Therefore, each muscle layer functions as asyncytium; that is, when an action potential is elicited anywhere within the muscle mass, it generally travels in all direc-tions in the muscle.The distance that it travels depends on the excitability of the muscle; sometimes it stops after only a few millimeters and at other times it travels many centimeters or even the entire length and breadth of the intestinal tract.
Also, a few connections exist between the longitu-dinal and circular muscle layers, so that excitation of one of these layers often excites the other as well.
Electrical Activity of Gastrointestinal Smooth Muscle
The smooth muscle of the gastrointestinal tract is excited by almost continual slow, intrinsic electrical activity along the membranes of the muscle fibers. This activity has two basic types of electrical waves: (1) slow waves and (2) spikes, both of which are shownin Figure 62–3. In addition, the voltage of the resting membrane potential of the gastrointestinal smooth muscle can be made to change to different levels, and this too can have important effects in controlling motor activity of the gastrointestinal tract.
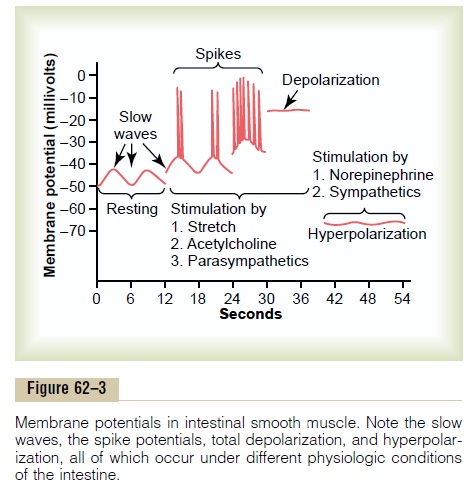
Slow Waves. Most gastrointestinal contractions occurrhythmically, and this rhythm is determined mainly by the frequency of so-called “slow waves” of smooth muscle membrane potential. These waves, shown in Figure 62–3, are not action potentials. Instead, they are slow, undulating changes in the resting membrane potential. Their intensity usually varies between 5 and 15 millivolts, and their frequency ranges in different parts of the human gastrointestinal tract from 3 to 12 per minute: about 3 in the body of the stomach, as much as 12 in the duodenum, and about 8 or 9 in the terminal ileum. Therefore, the rhythm of contraction of the body of the stomach usually is about 3 per minute, of the duodenum about 12 per minute, and of the ileum 8 to 9 per minute.
The precise cause of the slow waves is not com-pletely understood, although they appear to be caused by complex interactions among the smooth muscle cells and specialized cells, called the interstitial cells ofCajal, that are believed to act as electrical pacemakers for smooth muscle cells. These interstitial cells form a network with each other and are interposed between the smooth muscle layers, with synaptic-like contacts to smooth muscle cells. The interstitial cells of Cajal undergo cyclic changes in membrane potential due to unique ion channels that periodically open and produce inward (pacemaker) currents that may gen-erate slow wave activity.
The slow waves usually do not by themselves cause muscle contraction in most parts of the gastrointesti-nal tract, except perhaps in the stomach. Instead, they mainly excite the appearance of intermittent spike potentials, and the spike potentials in turn actually excite the muscle contraction.
Spike Potentials. The spike potentials are true actionpotentials. They occur automatically when the resting membrane potential of the gastrointestinal smooth muscle becomes more positive than about -40 milli-volts (the normal resting membrane potential in the smooth muscle fibers of the gut is between -50 and -60 millivolts).Thus, note in Figure 62–3 that each time the peaks of the slow waves temporarily become more positive than -40 millivolts, spike potentials appear on these peaks. The higher the slow wave potential rises, the greater the frequency of the spike potentials, usually ranging between 1 and 10 spikes per second. The spike potentials last 10 to 40 times as long in gas-trointestinal muscle as the action potentials in large nerve fibers, each gastrointestinal spike lasting as long as 10 to 20 milliseconds.
Another important difference between the action potentials of the gastrointestinal smooth muscle and those of nerve fibers is the manner in which they are generated. In nerve fibers, the action potentials are caused almost entirely by rapid entry of sodium ions through sodium channels to the interior of the fibers. In gastrointestinal smooth muscle fibers, the channels responsible for the action potentials are somewhat dif-ferent; they allow especially large numbers of calcium ions to enter along with smaller numbers of sodium ions and therefore are called calcium-sodium channels. These channels are much slower to open and close than are the rapid sodium channels of large nerve fibers. The slowness of opening and closing of the calcium-sodium channels accounts for the long dura-tion of the action potentials. Also, the movement of large amounts of calcium ions to the interior of the muscle fiber during the action potential plays a special role in causing the intestinal muscle fibers to contract, as we discuss shortly.
Changes in Voltage of the Resting Membrane Potential. Inaddition to the slow waves and spike potentials, the baseline voltage level of the smooth muscle resting membrane potential also can change. Under normal conditions, the resting membrane potential averages about -56 millivolts, but multiple factors can change this level. When the potential becomes less negative, which is called depolarization of the membrane, the muscle fibers become more excitable. When the poten-tial becomes more negative, which is calledhyperpo-larization, the fibers become less excitable.
Factors that depolarize the membrane—that is, make it more excitable—are (1) stretching of the muscle, (2) stimulation by acetylcholine, (3) stimula-tion by parasympathetic nerves that secrete acetyl-choline at their endings, and (4) stimulation by several specific gastrointestinal hormones.
Important factors that make the membrane poten-tial more negative—that is, hyperpolarize the mem-brane and make the muscle fibers less excitable—are (1) the effect of norepinephrine or epinephrine on the fiber membrane and (2) stimulation of the sympathetic nerves that secrete mainly norepinephrine at their endings.
Calcium Ions and Muscle Contraction. Smooth muscle con-traction occurs in response to entry of calcium ions into the muscle fiber. Calcium ions, acting through a calmodulin control mechanism, activate the myosin filaments in the fiber, causing attractive forces to develop between the myosin filaments and the actin filaments, thereby causing the muscle to contract.
The slow waves do not cause calcium ions to enter the smooth muscle fiber (only sodium ions).Therefore, the slow waves by themselves usually cause no muscle contraction. Instead, it is during the spike potentials, generated at the peaks of the slow waves, that signifi-cant quantities of calcium ions do enter the fibers and cause most of the contraction.
Tonic Contraction of Some Gastrointestinal Smooth Muscle.
Some smooth muscle of the gastrointestinal tract exhibits tonic contraction as well as or instead of rhyth-mical contractions. Tonic contraction is continuous, not associated with the basic electrical rhythm of the slow waves but often lasting several minutes or even hours. The tonic contraction often increases or decreases in intensity but continues.
Tonic contraction is sometimes caused by con-tinuous repetitive spike potentials—the greater the frequency, the greater the degree of contraction. At other times, tonic contraction is caused by hormones or other factors that bring about continuous partial depolarization of the smooth muscle membrane without causing action potentials. A third cause of tonic contraction is continuous entry of calcium ions into the interior of the cell brought about in ways not associated with changes in membrane potential. The details of these mechanisms are still unclear.
Related Topics