Chapter: Modern Pharmacology with Clinical Applications: Metabolism and Excretion of Drugs
Excretion in Other Body Fluids
EXCRETION IN
OTHER BODY FLUIDS
Sweat and Saliva
Excretion of drugs into sweat
and saliva occurs but has only minor importance for most drugs. The mechanisms
involved in drug excretion are similar for sweat and saliva. Excretion mainly
depends on the diffusion of the un-ionized lipid-soluble form of the drug
across the ep-ithelial cells of the glands. Thus, the pKa of the drug and the pH of the individual secretion
formed in the glands are important determinants of the total quantity of drug
appearing in the particular body fluid. It is not definitely established
whether active drug transport occurs across the ducts of the glands.
Lipid-insoluble compounds,
such as urea and glyc-erol, enter saliva and sweat at rates proportional to
their molecular weight, presumably because of filtration through the aqueous
channels in the secretory cell membrane. Drugs or their metabolites that are
excreted into sweat may be at least partially responsible for the dermatitis and
other skin reactions caused by some therapeutic agents. Substances excreted
into saliva are usually swallowed, and therefore their fate is the same as that
of orally administered drugs (unless expectora-tion is a major characteristic
of a person’s habits). The excretion of a drug into saliva accounts for the
drug taste patients sometimes report after certain com-pounds are given
intravenously.
Milk
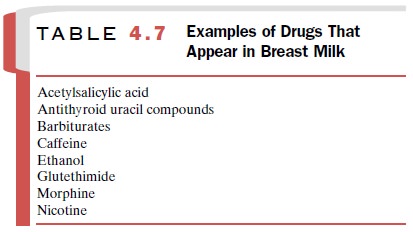
Many drugs in a nursing mother’s blood are detectable in her milk (Table 4.7). The ultimate
concentration of the individual
compound in milk will depend on many fac-tors, including the amount of drug in
the maternal blood, its lipid solubility, its degree of ionization, and the
extent of its active excretion. Thus, the physico-chemical properties that
govern the excretion of drugs into saliva and sweat also apply to the passage
of drugs into milk.
Since milk is more acidic (pH 6.5) than plasma, basic compounds (e.g., alkaloids, such as morphine and codeine) may be somewhat more concentrated in this fluid. In contrast, the levels of weak organic acids will probably be lower than those in plasma. In general, a high maternal plasma protein binding of drug will be associated with a low milk concentration.
A highly lipid-soluble drug should accumulate in milk fat.
Low-molecular-weight un-ionized water-soluble drugs will diffuse pas-sively
across the mammary epithelium and transfer into milk. There they may reside in
association with one or more milk components, for example, bound to protein
such as lactalbumin, dissolved within fat globules, or free in the aqueous
compartment. Substances that are not electrolytes, such as ethanol, urea, and
antipyrine, readily enter milk and reach approximately the same concentra-tion
as in plasma. Compounds used in agriculture also may be passed from cows to
humans by this route. Finally, antibiotics such as the tetracyclines, which can
function as chelating agents and bind calcium, have a higher milk than plasma
concentration.
Both maternal and infant
factors determine the final amount of drug present in the nursing child’s body
at any particular time. Variations in the daily amount of milk formed within
the breast (e.g., changes in blood flow to the breast) as well as alterations
in breast milk pH will affect the total amount of drug found in milk. In
addition, composition of the milk will be affected by the maternal diet; for
example, a high-carbohydrate diet will increase the content of saturated fatty
acids in milk.
The greatest drug exposure occurs when feeding be-gins shortly
after maternal drug dosing. Additional fac-tors determining exposure of the
infant include milk vol-ume consumed (about 150 mL/kg/day) and milk composition
at the time of feeding. Fat content is highest in the morning and then
gradually decreases until about 10 P.M. A longer feed usually results in exposure of
the infant to more of a fat-soluble drug, since milk fat con-tent increases
somewhat during a given nursing period.
Whether or not a drug
accumulates in a nursing child is affected in part by the infant’s ability to
elimi-nate via metabolism and excretion the ingested com-pound. In general, the
ability to oxidize and conjugate drugs is low in the neonate and does not
approach full adult rates until approximately age 6. It follows, there-fore, that
drug accumulation should be less in an older infant who breast-feeds than in a
suckling neonate.
Although abnormalities in
fetal organ structure and function can result from the presence of certain
drugs in breast milk, it would be quite inappropriate to deny the
breast-feeding woman appropriate and necessary drug therapy. A pragmatic
approach on the part of both the physician and patient is necessary. Breast-feeding should be discouraged when inherent drug toxicity
is known or when adverse pharmacological actions of the drug on the infant are
likely. Infant drug exposure can be mini-mized, however, through short
intermittent maternal drug use and by drug dosing immediately after
breast-feeding.
Related Topics