Chapter: Essentials of Psychiatry: Antidepressants
Antidepressants: Starting Doses
Starting
Doses
See Table
79.7 for usual therapeutic dosages.
First-generation Antidepressants
Tricyclic Antidepressants
TCAs are
usually begun at a relatively low dose. For the major-ity of TCAs, including
imipramine, amitriptyline, desipramine, maprotiline and doxepin, the initial
starting dose is in the range of 50 to 75 mg/day. Notable exceptions include
nortriptyline and protriptyline, which are more potent agents. In the case of
nortriptyline, the usual starting dose is 25 to 50 mg/day, and for
protriptyline, 10 to 15 mg/day (Schatzberg and Cole, 1991). The lower doses are
preferred in patients who are elderly. In the frail elderly, further dose
reductions may be needed (about one-half or less of the usual starting dose).
Once a
medication is initiated, it is gradually increased to a therapeutic level. A
number of strategies have been suggested for this increase. Most TCAs can be
increased to 150 mg/day by the second week, and then to a range of 300 mg/day
by the third or fourth week. This can be achieved through small daily increase
of 25 mg or weekly increase of 75 mg. Younger patients will tolerate larger and
more rapid increases, whereas the elderly benefit from smaller (25 mg/day) and
less frequent (every other day) increases with a lower target dose (150
mg/day).
For
nortriptyline, increases of 50 mg/week are usually tolerated in the young, with
the elderly requiring smaller increases (25 mg/week). Of particular interest is
nortriptyline’s therapeutic window: doses above and below a certain range
appear to be less effective. The effective range is approximately 50 to 150
mg/day. Some authors suggest a lower range (for example, from 30 to 100 mg
(Brotman et al., 1987); however,
plasma blood monitoring is a more accurate indicator of the proper level.
Monoamine Oxidase Inhibitors
Patients
taking MAOIs must adhere to a special diet to reduce the risk of a hypertensive
crisis (see Table 79.7) Phenelzine is usually begun at a dose of 30 mg/day. It
is increased by 15 mg after 3 days, then weekly to a target range of 45 to 90
mg/day. Tranylcypromine is started at 20 mg/day. It is increased by 10 mg after
3 days, with additional daily increases of 10 mg after 1 week, to a target
range of 30 to 60 mg/day. Isocarboxazid is usually begun at 20 mg/day. It is
titrated in a manner similar to tranylcypromine to a target of 30 mg/day.
Schatzberg and Cole (1991) suggested that most patients require doses in the
higher range, and that some may require doses above the normally recommended
limits (e.g., phenelzine at 120 mg/day tranylcypromine at 110 to 130 mg/day,
and isocarboxazid at 50 mg/day).
Second-generation Antidepressants
Serotonin Reuptake Inhibitors
Although
dosing strategies are less well understood with these agents, the wisest choice
is to start a patient at the lowest effective dose and increase as indicated by
clinical response. Reasonable doses are 20 mg/day for fluoxetine, 50 mg/day for
sertraline, 20 mg/day for paroxetine and citalopram. For children, adolescents,
the elderly and patients who find medications generally difficult to tolerate,
50% reductions in these doses are reasonable starting doses.
A number
of studies have shown increasing response with increasing doses of SSRIs
(Leonard, 1993), but the dropout rate due to side effects also increases with
increasing dose. Fluoxetine, paroxetine and citalopram should be started at a
dose of 10 or 20 mg for 3 weeks (20 mg for a normal healthy adult, 10 mg for
patients who are young, elderly, or particularly sensitive to medications),
after which they can be increased in 10 or 20 mg increments to a dose of 40
mg/day if there is no response. A maximum dose of 60 mg/day of fluoxetine is
recommended for the treatment of depression. A similar strategy can be used for
sertraline, which can be begun at 25 to 50 mg, and increased in 25 to 50 mg
increments to a target dose of 50 to 150 mg. Other disorders, particularly OCD
and bulimia nervosa, may require 80 mg/day or more for maximal effect. The
issue of dosage for SSRIs remains complicated, as some studies have suggested
that fluoxetine may not have a linear dose–response curve; some patients may
respond better to lower doses of the medication, such as 10 mg/day (Leonard,
1993). Other studies have documented responses to fluoxetine at incredible
doses and blood levels (320 mg/day and over 2000 ng/mL, respectively) without
adverse effects (Stoll et al., 1991).
As with
tricyclic medications, there is a significant delay between initiation of
medication and response, and there is no reason to believe that increasing the
dose hastens response.
Other Second-generation Antidepressants
Trazodone
is generally dosed in a manner similar to TCAs, with starting doses of 50 to 75
mg/day, and target ranges of 150 to 300 mg/day, with doses not exceeding 400
mg/day in outpatients and 600 mg/day in inpatients. Unlike many of the TCAs,
trazo-done’s short half-life requires divided doses, usually twice daily.
Bupropion,
like trazodone, requires divided doses. It is available in a short acting form
that requires three times a day dosing, or a longer acting form that allows
twice-daily dosing. It should be begun at 100 mg b.i.d., and increased to a
target of 300 mg/day after a few days. The recommended dose of the medication
is 300 mg/day; however, patients not responding to that dose can be increased
to 450 mg/day. Patients should be in-structed to avoid taking more than 150 mg
in a single dose. In the elderly, a usual starting dose is 75 mg/day of the
shorter acting preparation. This is then increased to 75 mg b.i.d.
Third-generation Antidepressants
Venlafaxine
It is
currently available in a slow release preparation that ena-bles once-daily
dosing. Venlafaxine is usually begun at a dose of 37.5 mg and is increased
within half to 1 week to a dose of 75 mg. If further increases are needed, it
can be titrated at a rate of 75 mg every 4 days or more. Though a maximum dose
of 225 mg per day is recommended by the manufacturer, doses as much as 300 to
450 mg/day have been employed to good effect in some patients.
Duloxetine
It is
available in 20, 30, and 60 mgm capsules. Starting dose is usually 20 mg twice
a day. Maximum recommended effective dose is 60 mgm/day.
Mirtazapine
Adults should be started on a dose of 15 mg/day. It is usually given as a before bedtime dose. The dosage generally needs to be increased in 15-mg intervals every half to 1 week to a target dose. The effective dose is usually between 15 and 45 mg/day; however, higher doses, such as 60 mg have been useful in some patients.
Nefazodone
Nefazodone
is given in twice-daily doses. Patients can be started at a dose of 100 mg
b.i.d. and increased at a rate of 100 to 200 mg a week. The recommended
effective dose is 300 to 600 mg/day. Some clinical experience suggests that
once-daily doses (given at night) are acceptable for some patients (Marathe et al., 1996).
Therapeutic Drug Monitoring
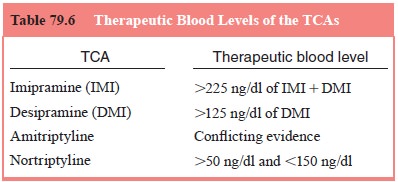
Although
blood levels are available for many antidepressants, those for imipramine,
desipramine, and nortriptyline have been best established (see Table 79.6).
Imipramine and desipramine appear to have a curvilinear dose–response curve
with an opti-mal range of 150 to 300 ng/mL. Nortriptyline appears to have a
therapeutic window in the range of 50 to 150 ng/mL (Preskorn et al., 1993). These blood levels are
nominal, as some patients do respond
above or below these ranges, and blood level monitoring should not be a
substitute for clinical observation.
Drug
levels have not been well established for the MAOIs and the serotonin reuptake
inhibitors.
Antidepressant Augmentation
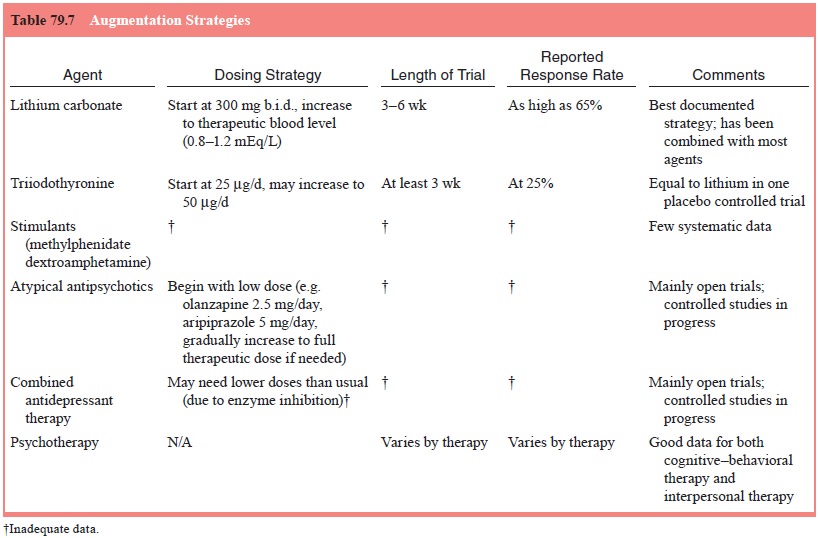
Typical
augmentation strategies (Table 79.7) include the addition of lithium carbonate,
thyroid hormone, or a stimulant. These may be considered when response is
inadequate to initial treatment using an adequate dose for an adequate time of
a single agent.
Changing to a New Agent
For the
patient who shows no response or whose condition dete-riorates during therapy,
the physician should initiate a new trial of an alternative single agent. There
remains some debate as to what type of agent should be used next. Some studies
have suggested that patients who do not respond to one SSRI may respond to
another (Thase et al., 1997).
However, the most convincing study continues to support the more commonly held
belief that it is best to switch to an agent of a different class, and
approximately 50% of patients unresponsive to a first trial respond to an
antidepressant of a differ-ent class (Phillips and Nierenberg, 1994; Thase et al., 2002).
When the switch involves an MAOI, sufficient time must be given for medication clearance. Although seldom used, MAOIs may be very effective in patients not responsive to other classes of antide-pressants (McGrath et al., 1993). Generally, 10 to 14 days for either medication is required for clearance of TCAs and MAOIs. Fluoxet-ine requires a much longer period – 6 weeks – whereas sertraline and paroxetine require about 2 weeks when switching to an MAOI.
Related Topics