Chapter: Clinical Cases in Anesthesia : Bradycardia and Hypertension
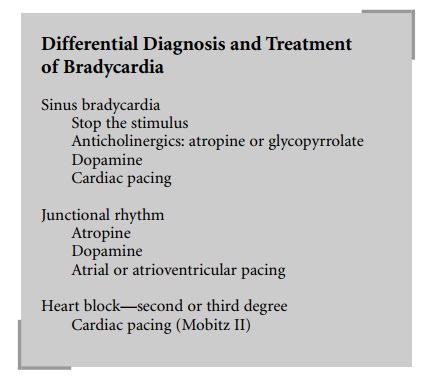
What is the differential diagnosis of bradycardia? What is the treatment for the different types of bradycardia?
What is
the differential diagnosis of bradycardia? What is the treatment for the
different types of bradycardia?
Bradycardia is said to exist when the heart
rate is less than 60 beats per minute. Bradydysrhythmias are usually
noncardiogenic in etiology, reflecting stimuli such as increased vagal tone,
drug side-effects, hypoxemia, and hypercarbia. The bradycardia may be either a
sinus brady-cardia, which is almost always benign, junctional rhythm, or
second- and third-degree atrioventricular blocks, which require a greater
sophistication in diagnosis and management.
Sinus bradycardia is usually well tolerated in
the absence of hypovolemia, systemic vasodilation and myocardial
hypocontractility. The treatment for sinus bradycardia is directed at removing
the cause. Surgical stimulation that results in increased vagal tone, such as
the oculocardiac reflex or peritoneal traction, should be stopped. Medications
that cause bradycardia, such as phenylephrine and fentanyl, should be replaced
by alterna-tive drugs or combined with a vagolytic drug (e.g., pan-curonium).
In the event that removing the stimulus cannot be accomplished or is
ineffective and there is a direct hemodynamic consequence of the bradycardia,
atropine 0.4–1.0 mg intravenously (IV) or glycopyrrolate in incre-ments of 0.2
mg IV may be administered. Glycopyrrolate may be preferable because it is
longer acting and is less likely to induce severe tachycardia. If necessary, a
dopamine infusion of 5–10 μg/kg/min can be used to increase the heart
rate. Isoproterenol is now rarely used because of the concomitant potent
vasodilation that can lead to severe hypotension. As a last resort,
transcutaneous or transvenous pacing may be required.
Junctional rhythms are due to decreased
automaticity of or damage to the sinus node. Cells further down the path-way
leading to the bundle of His take over but with a lower heart rate. The p waves
on electrocardiogram (ECG) are morphologically different from those seen on an
ECG recorded when the patient was in sinus rhythm. Depending on the level of
escape focus, the PR interval can be shortened or the p waves can be seen
within the QRS complex. Junctional rhythms are often seen with volatile
anesthetics, especially halothane, and after cardiac surgery. They are usually
benign and well tolerated, unless the loss of atrial “kick” leads to a
significant decrease in cardiac output, as in patients with diastolic
dysfunction and impaired ven-tricular filling. Atropine or dopamine can be used
to restore sinus node activity. If this fails, atrial or atrioven-tricular (AV)
pacing may be necessary.
Second-degree AV block may be further
classified into two major groups. Mobitz I (Wenckenbach) block is
char-acterized by a progressive increase in the PR interval result-ing in a
periodic failure to transmit the atrial impulse. The cause is usually an
intrinsic heart disease involving the AV node or digitalis toxicity. Because
the AV node is usually supplied by the right coronary artery, this dysrhythmia
commonly complicates inferior wall myocardial infarc-tions. It is usually a
benign and self-limited problem rarely requiring treatment. Mobitz II AV block
originates below the AV node and is characterized by a failure of atrial
depo-larization to conduct. This failure to conduct may occur in an
unpredictable manner or in a manner characterized by the “dropping” of every
other or every third beat, respec-tively termed 2:1 and 3:1 block. Importantly,
the PR inter-val for the conducted beats remains constant. Progression to
complete heart block is frequent and pacemaker inser-tion is usually necessary.
Third-degree block is almost always pathologic
and is characterized by a dissociation of the atrial depolarization and
ventricular response. Blockage may occur within or below the AV node. Blockage
within the node will present with narrow complex junctional rhythm usually at a
rate of 40–60 beats per minute. Blockage below the node, so-called infranodal
block, will present with a wide complex rhythm usually at a rate of 30–45 beats
per minute. Treatment will entail transcutaneous or transvenous pacing when
there is hemodynamic compromise. Blockage within the AV node may be transient
and, with close observation, permanent pacemaker placement may not be
necessary.
Related Topics