Chapter: Clinical Cases in Anesthesia : Bradycardia and Hypertension
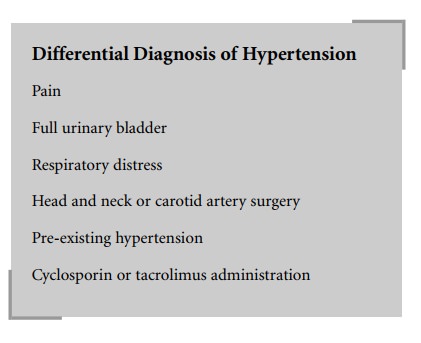
What is the differential diagnosis of postoperative hypertension?
What is
the differential diagnosis of postoperative hypertension?
Postoperative hypertension is an extremely
common finding, even in patients with no previous history of hyper-tension. The
most common cause is pain. The blood pres-sure should normalize as pain is
controlled with analgesics. Other common causes include: (1) a full urinary
bladder, which should be suspected after any prolonged procedure or
administration of large amounts of intravenous fluids in a patient without a
bladder catheter, (2) respiratory dis-tress, especially when there is
hypercapnia, (3) head and neck or carotid artery surgery, with carotid sinus
denerva-tion, and (4) cyclosporin or tacrolimus administration in patients
undergoing transplantation. Of course, a previous history of hypertension
should always be taken into account, especially if the patient did not take
their antihy-pertensive medication(s) on the day of surgery.
The presence of a combined bradycardia and
hyperten-sion in a patient who had a craniotomy leads one to suspect a primary
neurologic event causing what is known as the Cushing response or Cushing’s
triad. This consists of an increase in systemic blood pressure, a reflex
bradycar-dia, and bradypnea, and occurs when there is an elevation in
intracranial pressure. In this situation, hypertension should not be
aggressively treated because it is a comp-ensatory mechanism in an attempt to
maintain cerebral perfusion pressure. Rather, measures should be taken to
control intracranial pressure (head elevation, mannitol, hyperventilation,
possibly cerebrospinal fluid drainage after neurosurgical consultation).
Diagnostic imaging should be obtained to delineate the need for neurosurgical
intervention.
Related Topics