Chapter: Clinical Cases in Anesthesia : Intracranial Mass, Intracranial Pressure, Venous Air Embolism, And Autoregulation
What is cerebral autoregulation?
What is cerebral autoregulation?
Cerebral autoregulation is the control process
by which cerebral blood flow (CBF) is maintained constant over a wide range of
cerebral perfusion pressures (CPP) (Figure 17.1). CPP represents the difference
between mean arterial pres-sure (MAP) and ICP. Autoregulation adjusts cerebral
vessel caliber as CPP changes. Normal CBF is 45–65 ml/100 g of brain tissue per
minute. It is coupled to alterations in cere-bral metabolic rate, which is
linked to oxygen consumption (CMRO2). CBF parallels the changes in
CMRO2. Several parameters affect CBF.
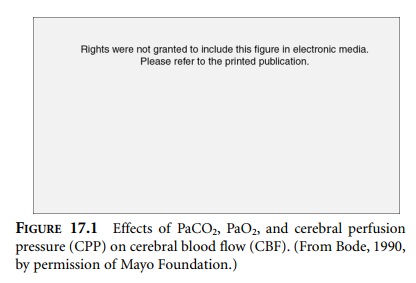
Autoregulation maintains CBF between a CPP of
50 and 150 mmHg. Below 50 mmHg, cerebral blood vessels achieve maximal
dilation; resistance to flow is low; and CBF falls in direct proportion to CPP.
Chronically hypertensive patients undergo an upward shift of autoreg-ulation to
higher perfusion pressures. Consequently, these patients require higher CPP to
maintain normal CBF. At the upper level of autoregulation, cerebral blood
vessels are maximally constricted, and CBF will rise linearly with increasing
CPP. Integrity of the blood–brain barrier is lost at these high pressures;
transudation of fluid occurs; and cerebral edema forms. Autoregulatory compensation
generally occurs over 1–3 minutes.
The
second parameter affecting CBF is arterial carbon dioxide tension (PaCO2).
Increasing levels of PaCO2 produce elevated levels of extracellular
hydrogen ion concen-trations, which induce cerebral vessel smooth muscle
relaxation and vasodilation. Consequently, cerebral vascular resistance falls,
increasing CBF by as much as twofold. This effect plateaus at a PaCO2
of approximately mmHg. Conversely, decreasing PaCO2 increases
cere-bral vasoconstriction and CBF decreases. At a PaCO2 of mmHg,
cerebral vasoconstriction is maximal and CBF decreases by 50%. Further
decreases in PaCO2 have no greater vacoconstricting influence. These
physiologic principles remain in effect for several hours, after which cerebral
spinal fluid (CSF) bicarbonate levels drop to compensate for the induced CSF
alkalosis. Once CSF pH returns toward normal, respiratory alkalosis no longer
provokes cerebral vasoconstriction. The PaCO2 response at the limits
of autoregulation can be blunted. If CPP is low and cerebral vessels are
maximally dilated, lowering PaCO2 will have little beneficial effect
on cerebral vascular resistance.
The third parameter affecting CBF is arterial
oxygen tension (PaO2). At a PaO2 below 50 mmHg, CBF rises
linearly with falling PaO2. Local accumulation of acidic metabolites
such as lactate results in cerebral vasodilation. In contradistinction,
hyperoxia has no effect on cerebral vascular tone.
Related Topics