Chapter: Clinical Cases in Anesthesia : Intracranial Mass, Intracranial Pressure, Venous Air Embolism, And Autoregulation
How do anesthetic agents and vasoactive drugs affect cerebral blood flow (CBF) and ICP?
How do
anesthetic agents and vasoactive drugs affect cerebral blood flow (CBF) and
ICP?
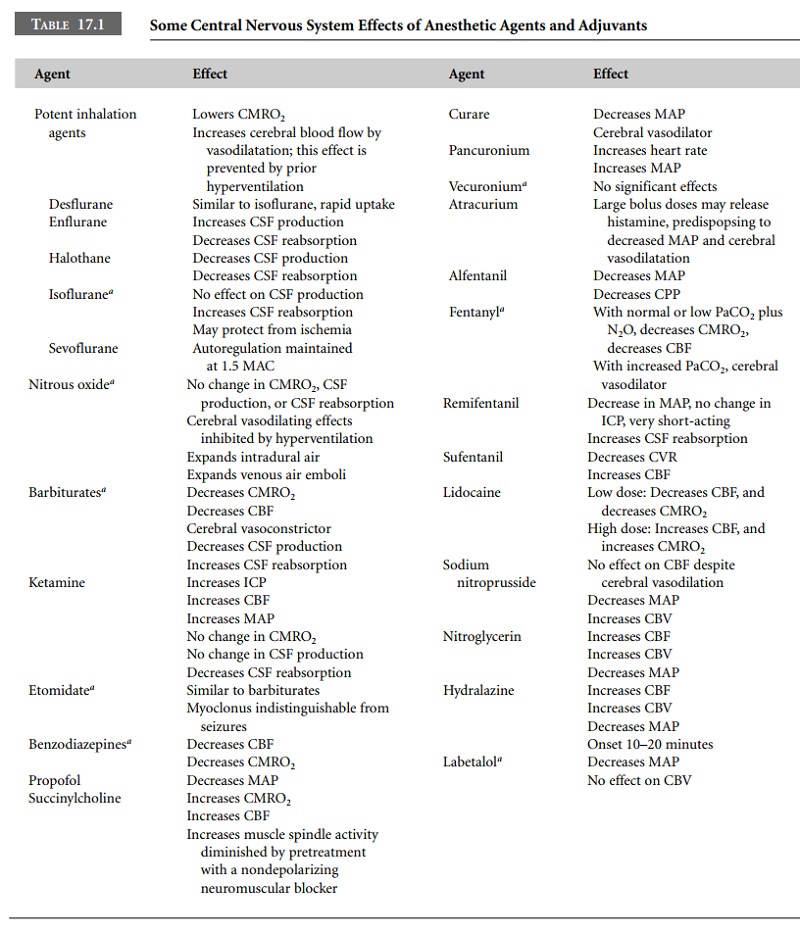
The effects of anesthetic agents and vasoactive
drugs are multifactorial (Table 17.1). They are described assuming nor-mal
brain anatomy and physiology, which is not commonly the situation for the
neurosurgical patient. The potent inhaled anesthetics are generally cerebral
vasodilators, which attenuate cerebral autoregulation. Inhalation anesthetics
pro-duce increases in CBF in a dose-dependent manner while producing
progressive depression of cerebral metabolism. The mechanism by which
inhalation anesthetics produce vasodilation is not clearly understood.
Mechanisms that par-tially explain the vasodilation include effects on nitric
oxide (NO) and ATP-dependent potassium channels.
Isoflurane increases CBF in a dose-dependent
fashion, but increases in subcortical CBF are greater than neo-cortical. CO2
reactivity is maintained but is greater in the awake state. Autoregulation is
adequately maintained at 1 MAC (minimal alveolar concentration) but is
progres-sively impaired by higher concentrations. Sevoflurane has very similar
CBF effects to isoflurane, although it appears to produce slightly less
vasodilation and autoregulation in humans is maintained up to 1.5 MAC.
Desflurane produces an increase in CBF similar to that seen with isoflurane but
greater than that seen with sevoflurane at >1 MAC. Autoregulation is
progressively abolished as the dose increases. Nitrous oxide (N2O)
is used in many neurosurgical anesthetics. Although it is a cerebral
vasodilator, this effect is diminished by hyperventilation, barbiturates, and
moderate concentrations of potent inhalation agents. When adminis-tered on its
own, N2O increases both CBF and metabolism. However, when added to
the background of another anes-thetic, it increases CBF without changing
metabolism.
Most of the intravenous anesthetics are
cerebral vaso-constrictors and maintain the relationship between CMRO2
and CBF. Barbiturates, notably thiopental, reduce CMRO2 primarily
and CBF secondarily. Thiopental acts as a cerebral vasoconstrictor. CO2
reactivity is maintained but is quanti-tatively reduced compared with the awake
state. Cerebral autoregulation is also maintained intact. Thiopental is an
excellent drug to acutely lower ICP; however, amounts suf-ficient to induce an
isoelectric electroencephalogram (EEG) can produce significant hemodynamic
side-effects.
Ketamine causes a significant rise in CBF
without an important effect on metabolic rate. It is not considered a wise
choice in the neurosurgical setting. However, small to moderate doses in a
background of volatile anesthetic or intravenous infusion have not been shown
to be signifi-cantly harmful. The trauma patient with hypovolemia and
concurrent injuries may be a suitable candidate for keta-mine as blood pressure
and CPP may be more easily main-tained. Etomidate behaves similarly to
thiopental and is an appropriate induction agent for patients who cannot
tolerate the hemodynamic effects seen with thiopental. Myoclonus, which occurs
after etomidate administration, may be difficult to differentiate from seizure
activity. Benzodiazepines offer beneficial effects on elevated ICP by lowering
CBF and diminishing CMRO2, without meaningful effects on CSF
dynamics.
Propofol is a short-acting intravenous agent
used for induction and maintenance of anesthesia. It appears to main-tain the
relationship between CBF and CMRO2. Propofol does not cause cerebral
vasodilation and does not interfere with the normal response to PaCO2.
It can be used to sup-plement anesthesia during long operations or as part of a
total intravenous technique. It is particularly useful for, and may be a good
choice for, neurodiagnostic procedures, keeping in mind that it produces
dose-dependent decreases in blood pressure.
Muscle relaxants have no direct intracerebral
effects because they do not cross the BBB. Nevertheless, they possess indirect
effects because of their actions in the periphery, which are sometimes
significant. There is clear evidence from both experimental animals and humans
that succinylcholine can increase ICP under conditions of intracranial
hypertension. The magnitude of the increase is typically small and transient.
It has been shown in humans that ICP changes caused by succinylcholine can be
blocked by preadministration of a defasciculating dose of a non-depolarizing
relaxant. A probable mechanism is the massive fasciculation-induced afferent
barrage from muscle spin-dles to the brain that causes transient increases in
meta-bolic rate and coupled increases in CBF. The decision to use this agent is
determined by the need to rapidly secure the airway. Pretreatment with a small
dose of a nondepo-larizing agent is helpful and recommended.
The nondepolarizing agents such as vecuronium,
rocuronium, and cisatracurium have no significant hemo-dynamic or ICP effects.
There is clear evidence that the duration of action of nondepolarizing muscle
relaxants is reduced by a variety of anticonvulsant medications. The mechanism
remains unclear. Most patients requiring craniotomy are being treated with
anticonvulsants and thus the nondepolarizing relaxant dosing regimen will
require alteration. Atracurium and cisatracurium seem to be largely resistant
to these effects, most likely because metabolism is achieved by Hoffman
elimination.
Opioids are known to produce respiratory depression,
which results in an increase in PaCO2. Consequently, opioids are
administered sparingly in the spontaneously breathing patient with cerebral
disease. Opioids at low doses produce very little effect on CBF provided PaCO2
is not allowed to rise. During controlled ventilation with normocapnia or
hypocapnia, opioids provide significant advantages. Independently, fentanyl
seems to have little effect on CBF or CMRO2, but when combined with
N2O it decreases CMRO2 and CBF, which is due to the
hemo-dynamic changes caused by this combination of anesthetic agents. It
increases the rate of CSF reabsorption without affecting its rate of
production. There is much controversy about how and whether opioids, such as
sufentanil and alfentanil, increase ICP. With cerebral autoregulation intact, a
drop in blood pressure results in a compensatory vasodi-lation to maintain CBF.
This increases cerebral blood volume and thus ICP. Remifentanil has become
increasingly used in neurosurgery for its rapid onset and offset, and titrat-ability
to changing stimuli. However, the lack of residual analgesia requires a plan
for postoperative pain relief as well as blood pressure control.
Sodium nitroprusside is a direct-acting smooth
muscle relaxant that produces arteriolar and venous dilatation. It is sometimes
used in neurosurgery for control of arterial blood pressure. Although it acts
as a cerebral vasodilator and decreases MAP, there is little effect on CBF.
However, cerebral blood volume is increased and ICP may be elevated. It is best
avoided if ICP is high. Thiopental, lidocaine or labetalol should be used
instead. Nitroglycerin is primarily a veno-dilator and coronary vasodilator
that acts by relaxing smooth muscle and works on the intracerebral venous
capacitance vessels. Hydralazine is a direct arteriolar vasodilator with an
onset time of 10–20 minutes. It increases cerebral blood volume and may
increase ICP when the dura is closed. Labetalol, a mixed α- and β-blocker, lowers MAP by lowering systemic
vascular resist-ance and depressing cardiac output. It has no direct effect on
cerebral blood vessels.
Related Topics