Chapter: Clinical Cases in Anesthesia : Respiratory Failure
What criteria are used to determine whether extubation will be successful?
After
several days in the SICU, the patient’s respira-tory status has improved. What
criteria are used to determine whether extubation will be successful?
Several criteria should be met to consider
extubation:
·
The
patient should be alert and cooperative on no sedation.
·
Muscular
strength should be adequate, with a negative inspiratory force (NIF) ≤ –25 cm H2O and/or
a forced vital capacity (FVC) ≥15 mL/kg.
·
The
hemodynamics should be stable, with no or minimal vasoactive infusions.
·
The PaO2
should be ≥60 mmHg on a FiO2 ≤0.5 and PEEP ≤5 cm H2O.
·
The PaCO2
should be ≤50 torr, or near the patient’s baseline.
·
The
patient should tolerate a trial of spontaneous venti-lation, either on the
respirator with a PS of 5–10 cm H2O or on a T-piece. No tachypnea,
dyspnea, tachycardia, hypertension, dysrhythmias, signs of myocardial ischemia,
or desaturation should be observed. Obtaining an ABG after 30 minutes of such a
trial does not add any further information to the clinical examination and the
pulse oximeter data.
Protocols driven by non-physician staff, such
as nurses or res-piratory therapists, have been shown to lead to significantly
earlier discontinuation of mechanical ventilation and should probably be the
rule.
Numerous criteria have been proposed to predict
successful extubation, but the most helpful may be the “rapid shallow breathing
index” or RSBI, calculated in a patient breathing spontaneously with a low PS.
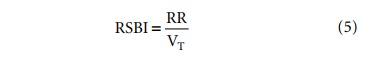
RR is the respiratory rate in breaths per
minute and VT is the tidal volume in liters. A value below 105
suggests that extubation will be successful.
Related Topics