Chapter: Obstetrics and Gynecology: Vulvovaginitis
Vulvovaginitis
Vulvovaginitis
Vulvovaginitis
is the spectrum of conditions that cause vaginal or vulvar symptoms such as itching,burning,
irritation, and abnormal discharge. Vaginal and vulvar symptoms are among the
most common reasons for patient visits to obstetrician–gynecologists.
Symptoms may be acute or subacute, and may range in intensity from mild to
severe. Vulvovaginitis may have important conse-quences in terms of discomfort
and pain, days lost from school or work, sexual functioning, and self-image.
Depend-ing on etiology, vulvovaginitis may also be associated with adverse
reproductive outcomes in pregnant and nonpreg-nant women.
Vulvovaginitis has a broad
differential diagnosis, and successful treatment frequently depends on
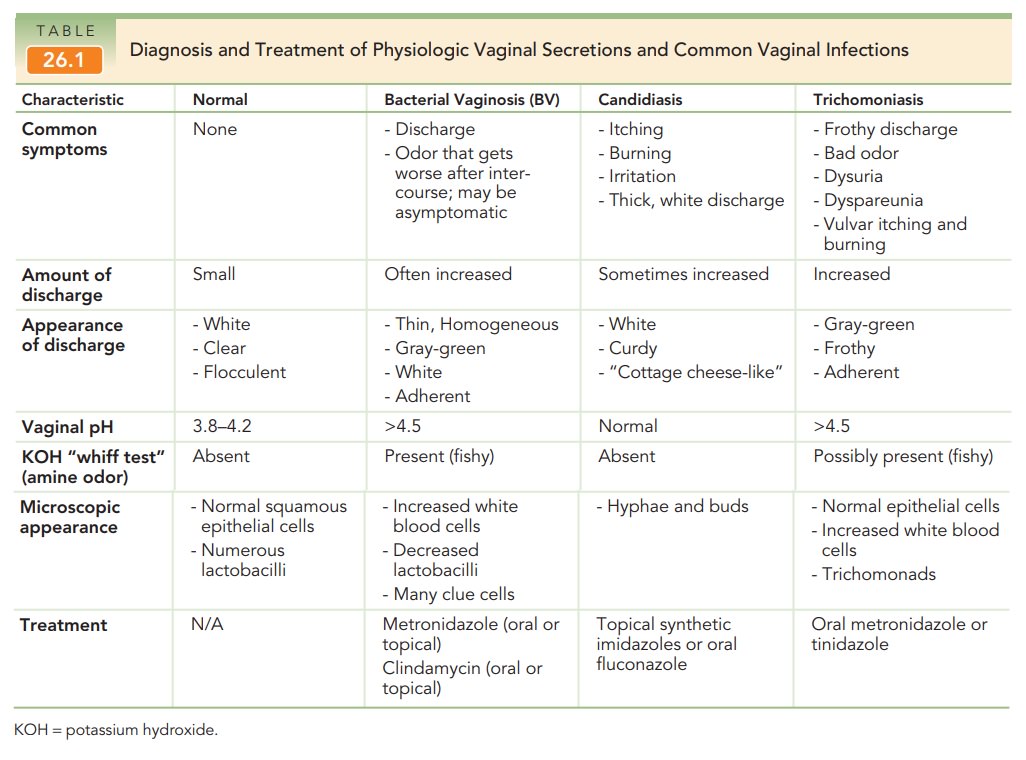
accurately iden-tifying its cause. The most common causes of vaginitis are
bacterial vaginosis (22%–50% of symptomatic women), vulvovaginal candidiasis
(17%–39%), and trichomoniasis (4%–35%). Common vaginal infections often present
with characteristic patterns (Table 26.1). The vulva and vagina are also sites
of symptoms and lesions of several sexually transmitted infections, such as
herpes genitalis, human pa-pillomavirus, syphilis, chancroid, granuloma
inguinale, lym-phogranuloma venereum, and molluscum contagiosum. It is
estimated that up to 70% of women with vaginitis remain undiag-nosed. In this
undiagnosed group, symptoms may be caused by a broad array of conditions,
including atrophic vaginitis, various vulvar dermatologic conditions, and
vulvodynia.
Although sexually transmitted and
other infections are common etiologies of vulvovaginitis, the patient’s
his-tory and symptoms may point to chemical, allergic, or other noninfectious
causes. Evaluation of women with vulvovaginitis should include a focused
history about the entire spectrum of vaginal symptoms, including change in
discharge, vaginal malodor, itching, irritation, burning, swelling,
dyspareunia, and dysuria. Questions about the location of symptoms (vulva,
vagina, anus), duration, the relation to the menstrual cycle, the response to
prior treat-ment including self-treatment and douching, and a sexual history
can yield important insights into the likely etiol-ogy. In patients with vulvar
symptoms, the physical exam-ination should begin with a thorough evaluation of
the vulva. However, evaluation may be compromised by pa-tient self-treatment
with nonprescription medications.
A variety of laboratory tests are
available to aid in di-agnosing the cause of vulvovaginitis. Samples obtained
dur-ing speculum examination can be tested for vaginal pH, amine (“whiff”)
test, and saline (wet mount) and 10% potas-sium hydroxide (KOH) microscopy.
Tests for diagnosing vaginal infection, such as rapid tests for enzyme activity
from bacterial vaginosis-associated organisms, Trichomonasvaginalis antigen, and point-of-care testing for DNA of Gardnerella vaginalis, Trichomonas
vaginalis, and Candida species
are also available, although the role of these tests in the proper management
of patients with vulvovaginitis is unclear. Depending on risk factors, DNA
amplification tests can be obtained for Neisseria
gonorrhoeae and Chlamydiatrachomatis.
Related Topics