Chapter: Obstetrics and Gynecology: Vulvovaginitis
Bacterial Vaginosis (BV): Vulvovaginal Candidiasis, Trichomonas Vulvovaginitis
BACTERIAL VAGINOSIS (BV)
Bacterial vaginosis (BV) is a
polymicrobial infection char-acterized by a lack of hydrogen peroxide-producing
lacto-bacilli and an overgrowth of facultative anaerobic organisms including G. vaginalis, Mycoplasma hominis,
Bacteroides species, Peptostreptococcus
species, Fusobacterium species, Prevotella species, and Atopobium vaginae.
Women with BV generally complain
of a “musty” or “fishy” odor with an increased thin gray-white to yellow
discharge. The discharge may cause mild vulvar irritation in approximately 25%
of the cases. The vaginal discharge is mildly adherent to the vaginal wall and
has a pH greater than 4.5.
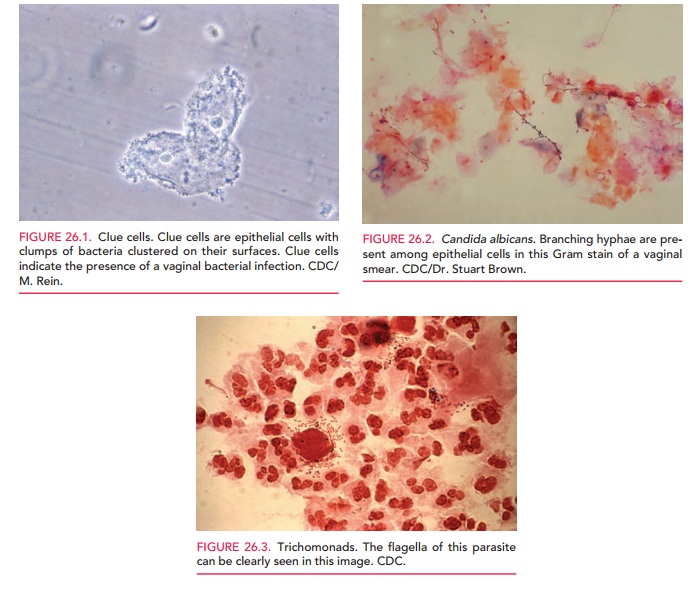
Microscopic examination made under saline wet mount shows a slight increase in white blood cells, clumps of bacteria, loss of normal lactobacilli, and characteristic “clue cells” (Fig. 26.1). These are epithelial cells with nu-merous coccoid bacteria attached to their surface, which makes their borders appear indistinct and their cytoplasm resemble “ground glass.” Because the bacteria that cause BV are part of the normal vaginal flora, the mere presence of these organisms is not diagnostic. The diagnosis of BV is defined by any three of the following four criteria: (1) ab-normal gray discharge, (2) pH greater than 4.5, (3) positive “whiff test,” and (4) the presence of clue cells.
BV may be treated with oral or
topical metronidazole or oral or topical clindamycin. Symptomatic pregnant
women can also be treated with these medications, as neither drug has been
shown to have teratogenic effects. Some studies have shown that screening for
and treatment of BV in women with high-risk pregnancies may reduce the incidence
of premature rupture of membranes (PROM) and preterm delivery. However, studies
do not confirm that universal BV screening and treatment in asympto-matic
pregnant women helps prevent adverse outcomes. In nonpregnant women, BV has
been associated with other in-fections, including pelvic inflammatory and
postoperative infections. It has also been associated with an increased risk of
acquisition of human immunodeficiency virus (HIV) and herpes simplex virus
(HSV). Although preoperative BV treatment may help prevent complications
stemming from postoperative infection, treatment for BV has not been shown to
decrease the risk of the HIV or HSV infection.
Vulvovaginal Candidiasis
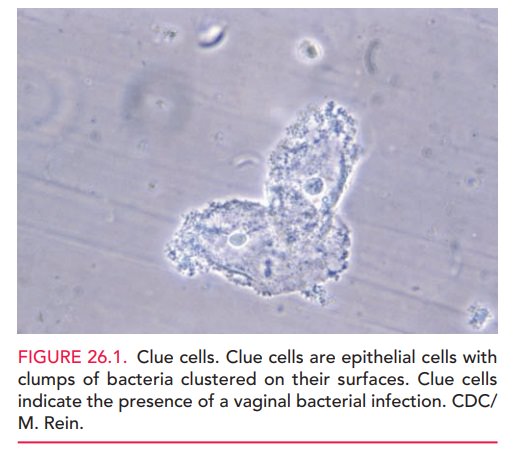
Vulvovaginal candidiasis is caused by ubiquitous airbornefungi. Approximately 90% of these infections are caused by Candida albicans (Fig. 26.2). The remaining cases are causedby Candida glabrata, Candida tropicalis, or Torulopsis glabrata. Candida infections generally do not coexist with other infections and are not considered to be sexually transmit-ted, although 10% of male partners have concomitant pe-nile infections. Candidiasis is more likely to occur in women who are pregnant, diabetic, obese, immunosuppressed, on oral contraceptives or corticosteroids, or have had broad-spectrum antibiotic therapy. Practices that keep the vaginal area warm and moist, such as wearing tight clothing or the habitual use of panty liners, may also increase the risk of Candida infections.
The most common presenting
complaint for women with candidiasis is itching, although up to 20% of women
may be asymptomatic. Burning, external dysuria, and dys-pareunia are also
common. The vulva and vaginal tissues are often bright red in color, and
excoriation is not un-common in severe cases. A thick, adherent “cottage
cheese” discharge with a pH of 4 to 5 is generally found. This dis-charge is
odorless.
Multiple studies conclude that a
reliable diagnosis can-not be made on the basis of history and physical
examina-tion alone. Over-the-counter (OTC) treatments are safe and effective,
but any woman who does not respond to OTC treatment or who has a recurrence
soon after treat-ment should be seen by a physician for a definitive
diagno-sis. Patients who have self-administered treatment with OTC medications
should be advised to stop treatment three days before their office visit.
Diagnosis requires either visualization of blastospores or pseudohyphae on
saline, or 10% KOH microscopy, or a positive culture in a sympto-matic woman.
The diagnosis can be further classified as uncomplicated or complicated
vulvovaginal candidiasis (Box 26.1). Latex agglutination tests may be of
particular use for non-Candida albicans
strains, because they do not demonstrate the pseudohyphae on wet prep.
Treatment of candida infections
is primarily with the topical application of one of the synthetic imidazoles,
such as miconazole, clotrimazole, butoconazole, or tercona-zole in cream or
suppository form placed intravaginally. Short-term oral therapy with low-dose
(150 mg) flucona-zole has become widely used. Pregnant women should be treated
with topical agents due to the increased risk of birth defects associated with
high doses (400 to 800 mg) of fluconazole.
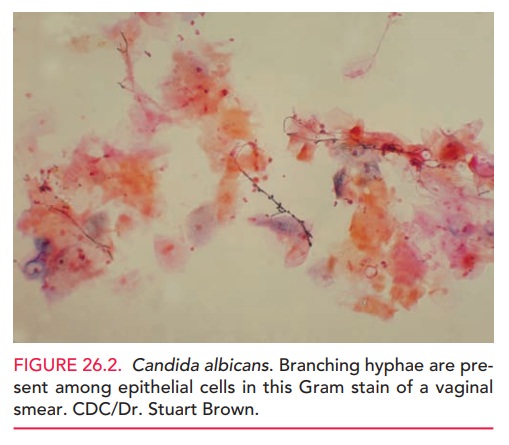
Box 26.1
Classification of Vulvovaginal Candidiasis
Although these agents are
associated with high cure rates, approximately 20% to 30% of patients
experience re-currences one month after treatment. Weekly therapy with fluconazole
for six months has been shown to be effective in preventing recurrent
candidiasis in 50% of women. Intermittent therapy with topical agents (weekly
or twice weekly) can also be used for prevention. T. glabrata is resis-tant to all azoles and may respond to therapy
with intra-vaginal boric acid capsules or gentian violet. Patients with
frequent recurrences should be carefully evaluated for pos-sible risk factors
such as diabetes or autoimmune disease. Prophylactic local therapy with an
antifungal agent should be considered when systemic antibiotics are prescribed.
Trichomonas Vulvovaginitis
T.
vaginalis is a flagellate protozoan that lives only in
thevagina, Skene ducts, and male or female urethra. The infec-tion can be
transmitted by sexual contact, but can also occur via fomites, and the organism
has been known to survive in swimming pools and hot tubs. Trichomoniasis is
associated with pelvic inflammatory disease (PID), endometritis, in-fertility,
ectopic pregnancy, and preterm birth, and it often coexists with other sexually
transmitted diseases and BV. It has also been shown to facilitate HIV
transmission.
Symptoms of trichomonas infection
vary from mild to severe and may include vulvar itching or burning, copious
discharge with rancid odor, dysuria, and dyspareunia. Although not present in
all women, the discharge associ-ated with trichomonas infections is generally
“frothy,” thin, and yellow-green to gray in color, with a pH above 4.5.
Examination may reveal edema or erythema of the vulva. Petechiae, or strawberry
patches, are classically de-scribed as present in the upper vagina or on the
cervix, but are actually found in only about 10% of affected patients. A
significant number of women with trichomoniasis are asymptomatic.
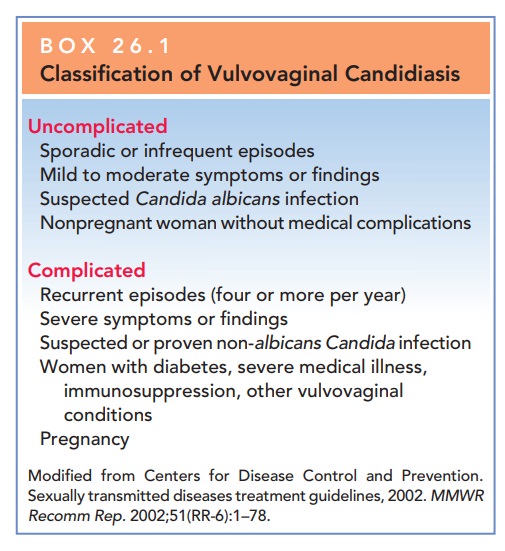
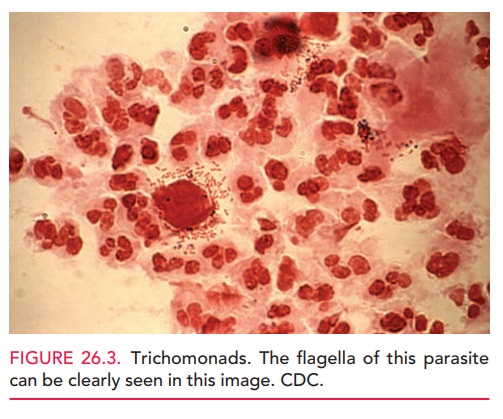
The diagnosis is confirmed by
microscopic examina-tion of vaginal secretions suspended in normal saline. This
wet smear will show large numbers of mature epithelial cells, white blood cells
(WBCs), and the trichomonas or-ganism (Fig. 26.3). A point-of-care test for
trichomonas antigens, the OSOM Trichomonas Rapid Test, has a sen-sitivity of
88.3% and specificity of 98.8% compared with culture. Women diagnosed with
trichomoniasis should also undergo screening for other STDs, especially
gonor-rhea and chlamydia.
Treatment of trichomonas
infections is with oral metronidazole or tinidazole. Treating sexual partners
of women with trichomoniasis is recommended, and individ-uals undergoing
treatment should avoid unprotected intercourse. Abstinence from alcohol use
when taking metronidazole is necessary to avoid a possible disulfiram-like
reaction. Trichomoniasis has been associated with preterm delivery, PROM, and
low birth weight. Pregnant patients should be treated, and metronidazole is
consid-ered safe for use during pregnancy. However, treatment may not prevent
these pregnancy complications.
Although follow-up examination of patients with tri-chomoniasis for test of cure is often advocated, they are usu-ally not cost-effective, except in the rare patient with a history of frequent recurrences. In these patients, reinfec-tion or poor compliance must be considered as well as the possibility of infection with more than one agent or other underlying disease. Infections with metronidazole-resistant T. vaginalis have been reported. Although absolute resistance is rare, relative resistance may be as high as 5%. These infections are treated with high doses of tinidazole.
Related Topics