Chapter: Modern Pharmacology with Clinical Applications: Antihypertensive Drugs
Vasodilators
VASODILATORS
The drugs discussed in this
section produce a direct re-laxation of vascular smooth muscle and thereby
their actions result in vasodilation. This effect is called direct because it does not depend on the
innervation of vascu-lar smooth muscle and is not mediated by receptors, such
as adrenoceptors, cholinoreceptors, or receptors for histamine, that are acted
on by classical transmitters and mediators.
The vasodilators decrease
total peripheral resistance and thus correct the hemodynamic abnormality that
is responsible for the elevated blood pressure in primary hypertension. In
addition, because they act directly on vascular smooth muscle, the vasodilators
are effective in lowering blood pressure, regardless of the etiology of the
hypertension. Unlike many other antihypertensive agents, the vasodilators do not inhibit the activity of the
sympathetic nervous system; therefore, orthostatic hypotension and impotence
are not problems. Additionally, most vasodilators relax arterial smooth muscle
to a greater extent than venous smooth muscle, thereby further minimizing
postural hypotension.
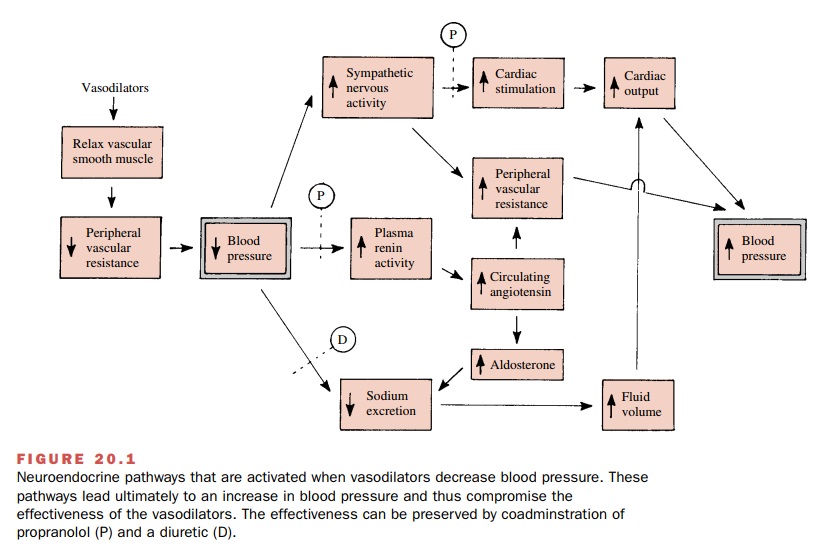
Although vasodilators would
appear to be ideal drugs for the treatment of hypertension, their
effective-ness, particularly when they are used chronically, is se-verely
limited by neuroendocrine and autonomic re-flexes that tend to counteract the
fall in blood pressure. How these reflexes compromise the fall in blood pres-sure
produced by the vasodilators is shown in Fig. 20.1. The diagram does not show
all of the possible interrela-tionships but rather is meant to draw attention
to the most prominent reflex changes.
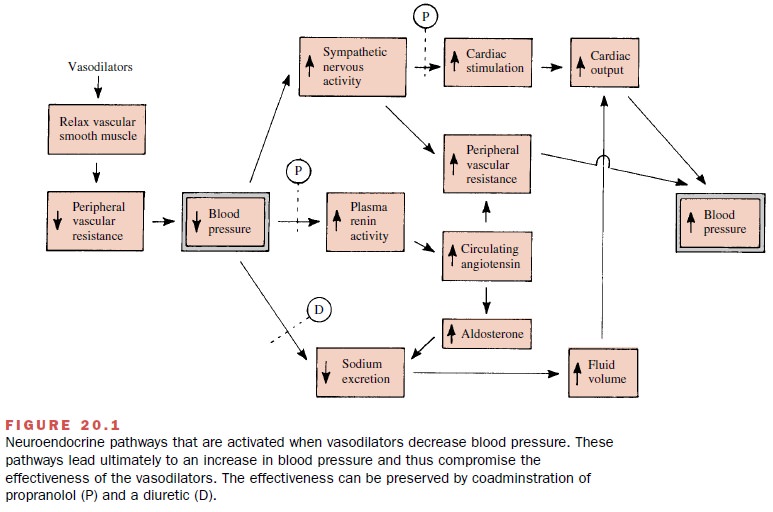
These reflexes include an augmentation of sympathetic nervous activity that leads to an increase in heart rate
and cardiac output. Large increases in cardiac output occurring as a result of
va-sodilator therapy will substantially counter the drug-induced reduction of
blood pressure. Increased reflex sympathetic input to the heart also augments
myocardial oxygen demand; this is especially serious in patients with coronary
insufficiency and little cardiac reserve.
Plasma renin activity is elevated after treatment with
vasodilators. The hyperreninemia appears to be due in part to enhanced sympathetic nervous activity. Elevated renin
levels lead to an increase in the concentration of circulating angiotensin, a
potent vasoconstrictor and thus an
increase in peripheral vascular resistance.
Thus, it seems that the lack
of sympathetic nervous system inhibition produced by the vasodilators, which is
advantageous in some ways, can also be a disadvantage in that reflex increases
in sympathetic nerve activity will lead to hemodynamic changes that reduce the
effective-ness of the drugs. Therefore,
the vasodilators are gener-ally inadequate as the sole therapy for
hypertension. However, many of the factors that limit the usefulness of the
vasodilators can be obviated when they are ad-ministered in combination with a β-adrenoceptor
antag-onist, such as propranolol, and a
diuretic. Propranolol reduces the
cardiac stimulation that occurs in response to increases in sympathetic nervous
activity, and the large increase in cardiac output caused by the vasodila-tors
will be reduced. Propranolol also reduces plasma renin levels, and that is an
additional benefit. The re-duction in NA+ excretion and the increase
in plasma vol-ume that occurs with vasodilator therapy can be re-duced by
concomitant treatment with a diuretic. These relationships are shown in Fig.
20.1.
Related Topics