Chapter: Microbiology and Immunology: Immunity
Types of Immunity
Types of Immunity
The main function of the immune system is to prevent or limit
infections by pathogenic microorganisms, such as bacteria, viruses, parasites,
and fungi. The recognition of microorganisms and for-eign substances is the
first event in immune responses of a host. The body’s defense mechanisms can be
divided into: (a) innate (natural)
immunity and (b) acquired (adaptive)
immunity.
Innate Immunity
Innate immunity is the resistance that an individual possesses by
birth. Innate immunity may be classified as (a) individual immunity, (b)
racial immunity, and (c) species
immunity.
Individual immunity: Individual immunity denotes
resis-tance to infection, which varies within different individuals in the same
race and species and is genetically determined. For example, if one homozygous
twin develops tuberculosis, there is a very high possibility that the other
twin will also develop tuberculosis. But in heterozygous twins, there is a very
low possibility of the other twin suffering from tuberculosis.
Racial immunity: Racial immunity denotes a
difference insusceptibility or resistance to infection among different races
within a same species. For example, races with sickle cell ane-mia prevalent in
Mediterranean coast are immune to infection caused by malaria parasite Plasmodium falciparum. This is due to a
genetic abnormality of erythrocytes, resulting in sickle-shaped erythrocytes
that prevent parasitization by P.
falciparum. Similarly, individuals with a hereditary deficiency of
glucose-6-phosphatase dehydrogenase are also less susceptible to infection by P. falciparum.
Species immunity: Species immunity denotes a
total or relativeresistance to a pathogen shown by all members of a particular
spe-cies. For example, chickens are resistant to Bacillus anthracis, rats are resistant to Corynebacterium diphtheriae, whereas humans are susceptible to
these bacteria. The exact reason for such type of immunity is not known.
◗
Factors influencing innate immunity
The factors that may influence innate immunity of the host include
age and nutritional status of the host.
Age: Extremes of age make an
individual highly susceptible tovarious infections. This is explained in part
by the immature immune system in very young children and waning immunity in
older individuals. The fetus-in-utero is usually protected from maternal
infections by the placental barrier. However, human immunodeficiency virus
(HIV), rubella virus, cytomeg-alovirus, and Toxoplasma
gondii cross the placental barrier and cause congenital infections.
Very old people are susceptible to suffer more than young people
from a disease (e.g., pneumonia) and have high mortal-ity. Measles, mumps,
poliomyelitis, and chicken pox are few examples of the diseases that cause more
severe clinical illness in adults than in young children. This may be due to
more active immune response in an adult causing greater tissue damage.
Nutritional status: Nutritional status of the
host plays animportant role in innate immunity. Both humoral and cell-mediated
immunities are lowered in malnutrition. Examples are:
·
Neutrophil activity is reduced, interferon response is decreased,
and C3 and factor B of the complement are decreased in protein–calorie
malnutrition.
·
Deficiency of vitamin A, vitamin C, and folic acid makes an
individual highly susceptible to infection by many microbial pathogens.
Hormonal levels: Individuals with certain
hormonal disordersbecome increasingly susceptible to infection. For example,
indi-viduals suffering from diabetes mellitus, hypothyroidism, and adrenal
dysfunction are increasingly susceptible to staphylococ-cal infection,
streptococcal infection, candidiasis, aspergillosis, zygomycosis and many other
microbial infections. Similarly, pregnant women are more susceptible to many
infections due to higher level of steroid during pregnancy.
◗
Mechanisms of innate immunity
Innate immunity of the host performs two most impor-tant functions:
it kills invading microbes and it activates acquired (adaptive) immune
processes. Innate immunity unlike adaptive immunity, however, does not have any
memory and does not improve after re-exposure to the same microorganism. The
innate immunity is primarily dependent on four types of defensive barriers: (a) anatomic barriers, (b) physiologic barriers, (c) phagocytosis, and (d) inflammatory responses.
Anatomic barriers: Anatomic barriers include
skin andmucous membrane. They are the most important components of innate
immunity. They act as mechanical barriers and prevent entry of microorganisms
into the body. The intact skin prevents entry of microorganisms. For example,
breaks in the skin due to scratches, wounds, or abrasion cause infection. Bites
of insects harboring pathogenic organisms (e.g., mosquitoes, mites, ticks,
fleas, and sandflies), introduce the pathogens into the body and transmit the
infection. Skin secretes sebum, which prevents growth of many microorganisms.
The sebum consists of lactic acid and fatty acids that maintain the pH of skin
between 3 and 5, and this pH inhibits the growth of most microorganisms.
Mucous membranes form a large part of outer cover-ing of
gastrointestinal, respiratory, genitourinary, and many other tracts of human
host. A number of nonspecific defense mechanisms act to prevent entry of
microorganisms through mucous membrane.
·
Saliva, tears, and mucous secretions tend to wash away potential
invading microorganisms, thereby preventing their attachment to the initial
site of infections. These secre-tions also contain antibacterial or antiviral
substances that kill these pathogens.
·
Mucus is a viscous fluid secreted by the epithelial cells of mucous
membranes that entraps invading microorganisms.
·
In lower respiratory tract, mucous membrane is covered by cilia,
the hair-like protrusions of the epithelial cell mem-branes. The synchronous
movement of cilia propels mucus-entrapped microorganisms from these tracts.
·
In addition, nonpathogenic organisms tend to colonize the
epithelial cells of mucosal surfaces. These normal flora generally compete with
pathogens for attachment sites on the epithelial cell surface and for necessary
nutrients.
Physiologic barriers: The physiologic barriers that
contributeto innate immunity include the following:
·
Gastric acidity is an innate physiologic barrier to infection
because very few ingested microorganisms can survive the low pH of stomach
contents.
·
Lysozyme, interferon, and complement are some of the soluble
mediators of innate immunity. Lysozyme has anti-bacterial effect due to its action
on the bacterial cell wall. Interferons are secreted by cells in response to
products of viral infected cells. These substances have a general antiviral
effect by preventing the synthesis of viral structural proteins. Complement is
a group of serum-soluble substances that when activated damage the cell
membrane.
·
There are certain types of molecules that are unique to microbes
and are never found in multicellular organisms. The ability of the host to
immediately recognize and com-bat invaders displaying such molecules is a
strong feature of innate immunity.
Phagocytosis: Phagocytosis is another
important defensemechanism of the innate immunity. Phagocytosis is a process of
ingestion of extracellular particulate material by certain specialized cells,
such as blood monocytes, neutrophils, and tis-sue macrophages. It is a type of
endocytosis in which invading microorganisms present in the environment are
ingested by the phagocytic cells. In this process, plasma membrane of the cell
expands around the particulate material, which may include whole pathogenic
microorganisms to form large vesicles called phagosomes.
Inflammatory responses: Tissue damage caused by a
woundor by an invading pathogenic microorganism induces a com-plex sequence of
events, collectively known as the inflamma-tory responses. The end result of
inflammation may be the activation of a specific immune response to the
invasion or clearance of the invader by components of the innate immune system.
The four cardinal features of inflammatory responses are rubor (redness), calor
(rise in temperature), dolor (pain),
and tumor (swelling).
Mediators of inflammatory reactions: Histamine, kinins,
acute-phase proteins, and defensin are the important mediators of inflammatory
reactions.
·
Histamine: It is a chemical substance
produced by a varietyof cells in response to tissue injury. It is one of the
principal mediators of the inflammatory response. It binds to recep-tors on
nearby capillaries and venules, causing vasodilata-tion and increased
permeability.
·
Kinins: These are other important
mediators of inflamma-tory response. They are normally present in blood plasma
in an inactive form. Tissue injury activates these small peptides, which then
cause vasodilatation and increased permeability of capillaries. Bradykinin also
stimulates pain receptors in the skin. This effect probably serves a protective
role because pain normally causes an individual to protect the injured area.
·
Acute-phase proteins: These include C-reactive
pro-teins and mannose-binding proteins that form part of the innate immunity.
These proteins are produced at an increased concentration in plasma during
acute-phase reaction, as a nonspecific response to microorganisms and other
forms of tissue injury. They are synthesized in the liver in response to
cytokines called proinflammatorycytokines, namely, interleukin-1 (IL-1),
interleukin-6 (IL-6), and tissue necrosis factor (TNF). They are called
pro-inflammatory cytokines because they enhance the inflam-matory responses.
·
Defensins: They are another important
component of theinnate immunity. They are cationic peptides that produce pores
in membrane of the bacteria and thereby kill them. These are present mainly in
the lower respiratory tract and gastrointestinal tract. The respiratory tract
contains b-defensins, whereas the gastrointestinal tract contains a-defensins. The a-defensins also exhibit
antiviral activ-ity. They bind to the CXCR4 receptors and block entry of HIV
virus into the cell. How these defensins differentiate microbes from some cells
is not known.
Adaptive (Acquired) Immunity
Adaptive immunity is also called acquired immunity, since the
potency of immune response is acquired by experience only. Differences between
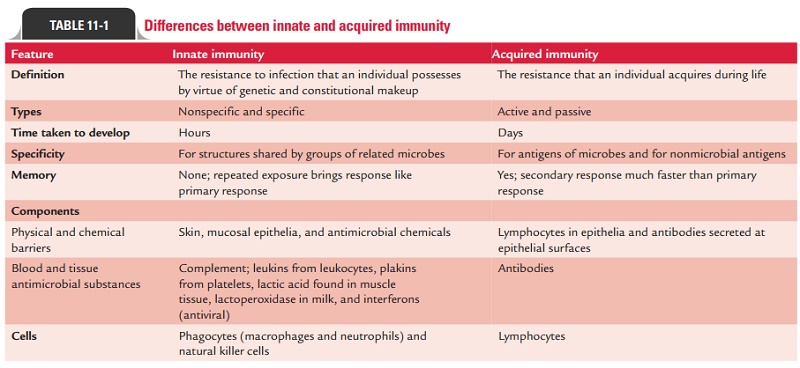
innate and acquired immunity are summarized in Table 11-1.
◗
Types of acquired immunity
Acquired immunity against a microbe may be induced by the host’s
response to the microbe or by transfer of antibodies or lymphocytes specific
for the microbes. It is of two types: activeimmunity
and passive immunity.
Active immunity
The immunity induced by exposure to a foreign antigen is called active
immunity. Active immunity is the resistance devel-oped by an individual
after contact with foreign antigens, e.g., microorganisms. This contact may be
in the form of:
·
clinical or subclinical infection,
·
immunization with live or killed infectious agents or their
antigens, or
·
exposure to microbial products, such as toxins and toxoids.
In all these circumstances, the immune system of the host is
stimulated to elicit an immune response consisting of antibod-ies and activated
helper T (TH) cells and cytotoxic T lympho-cytes/cells (CTLs).
Active immunity develops after a latent period, during which
immunity of the host is geared up to act against the microorganism. Hence it is
slow in onset, especially during this primary response. However, once the
active immunity develops, it is long-lasting and this is the major advantage of
the active immunity. The active immunity is of two types: natural active
immunity and artificial active immunity.
·
Natural active immunity:It is acquired by natural
clinicalor subclinical infections. Such natural immunity is long-lasting. For
example, individuals suffering from smallpox become immune to second attack of
the disease.
· Artificial active immunity: It is induced in individuals byvaccines. There is a wide range of vaccines available against many microbial pathogens. These may be live vaccines, killed vaccines, or vaccines containing bacterial products (Table 11-2).
Mediators of active immunity: Active immunity is mediatedby humoral immunity and cell-mediated immunity. These two types of immunities are mediated by different components of the immune system and function in different ways to kill different types of pathogens.
·
Humoral immunity: It is mediated by molecules in theblood and
mucosal secretions called antibodies. The anti-bodies are secreted by a subset
of lymphocytes known as B cells. The antibodies recognize microbial antigens, combine
specifically with the antigens, neutralize the infectivity of microbes, and
target microbes for elimina-tion by various effector mechanisms. Humoral
immunity is the principal defense mechanism against extracellular microbes.
·
Cell-mediated immunity: It is mediated by both activatedTH
cells and CTLs. Cytokines secreted by TH cells activate various
phagocytic cells, enabling them to phagocytose and kill microorganisms. This
type of cell-mediated immune response is especially important against a host of
bacte-rial and protozoal pathogens. CTLs play an important role in killing
virus-infected cells and tumor cells. They act by killing altered self-cells.
Differences between humoral and cell-mediated immunities are
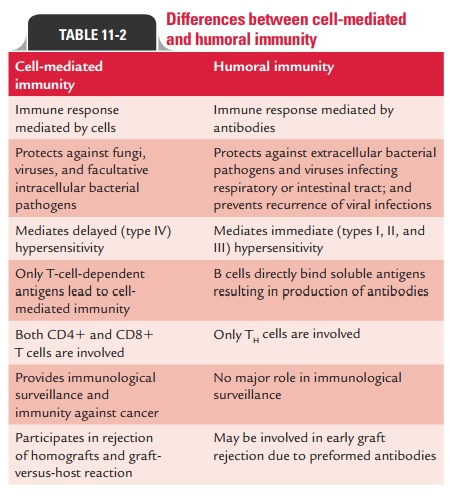
summarized in Table 11-2.
Antigen recognition: Antigens, which are generally
very largeand complex, are not recognized in their entirety by lympho-cytes.
Instead, both B and T lymphocytes recognize discrete sites on the antigens
called antigenic determinants, or epitopes. Epitopes are the immunologically
active regions on a com-plex antigen, the regions that actually bind to B-cell
or T-cell receptors.
B cells and T cells
differ in their mechanisms of antigen recognition. While B cells recognize the
antigen by interacting with the epitope on their own, T cells recognize the
antigen only when the epitope is “presented” by one of the specialized
antigen-presenting cells. Once the antigen has been recognized, these cells
then go on to diversify by several intricate mecha-nisms. This diversification
helps in conferring the specificity, one of the cardinal characteristics of the
immune system.
Major histocompatibility
complex (MHC): It is a largegenetic complex with multiple loci. The MHC loci
encode two major classes of membrane-bound glycoproteins: class I and class II
MHC molecules. Class II molecules present antigens to the TH cells,
while class I molecules do the same for CTLs. In order for a foreign protein
antigen to be recognized by a T cell, it must be degraded into small antigenic
peptides that form complexes with class I or class II MHC molecules. This
con-version of proteins into MHC-associated peptide fragments is called antigen
processing and presentation.
Passive immunity
When immunity is conferred by transfer of serum or lympho-cytes
from a specifically immunized individual, it is known as passive immunity. This is
a useful method for conferring resis-tance rapidly, i.e., without waiting for
the development of an active immune response. Passive immunity may be natural
or artificial.
Natural passive immunity: It is observed when IgG is
passedfrom mother to fetus during pregnancy. This forms the basis of prevention
of neonatal tetanus in neonates by active immu-nization of pregnant mothers. It
is achieved by administering tetanus toxoid to pregnant mothers during the last
trimester of pregnancy. This induces production of high level of antibod-ies in
mother against tetanus toxin, which are subsequently transmitted from mother to
fetus through placenta. The anti-bodies subsequently protect neonates after
birth against the risk of tetanus. Natural passive immunity is also observed by
passage of IgA from mother to newborn during breast feeding.
Artificial passive immunity: It is induced in an
individ-ual by administration of preformed antibodies, generally in the form of
antiserum, raised against an infecting agent. Administration of these antisera
makes large amounts of antibodies available in the recipient host to neutralize
the action of toxins.
The preformed antibodies against rabies and hepatitis A and B
viruses, etc. given during incubation period prevent replication of virus, and
hence alter the course of infection. Immediate availability of large amount of
antibodies is the main advantage of passive immunity. However, short lifes-pan
of these antibodies and the possibility of hypersensitiv-ity reaction, if
antibodies prepared in other animal species are given to individuals who are
hypersensitive to these animal globulins (e.g., serum sickness), are the two
noted disadvan-tages of passive immunity.
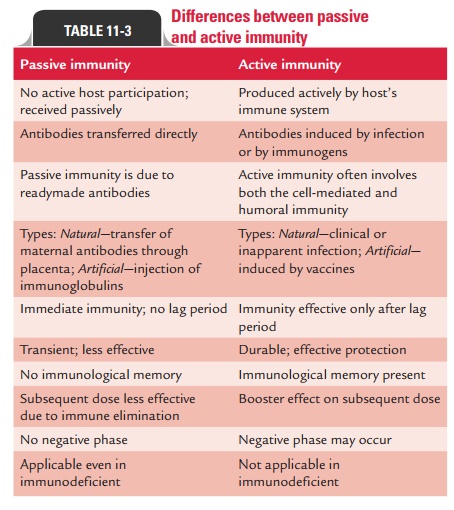
Differences between active and passive immunity are summarized in
Table 11-3.
Combined passive–active immunity is carried out by giving both
preformed antibodies (antiserum) and a vaccine to provide immediate protection
and long-term protection, respectively, against a disease. This approach is
followed for prevention of certain infectious conditions, namely, tetanus,
rabies, and hepatitis B.
Local Immunity
The immunity at a particular site, generally at the site of
invasion and multiplication of a pathogen, is referred to as local
immunity. Local immunity is conferred by secretory IgAantibodies in
various body secretions. These antibodies are produced locally by plasma cells
present on mucosal surfaces or in secretory glands. Natural infection or
attenuated live viral vaccines given orally or intranasally induces local
immunity at gut mucosa and nasal mucosa, respectively.
Herd Immunity
Herd immunity refers to an overall level of immunity in a commu-nity. Eradication of an infectious
disease depends on the devel-opment of a high level of herd immunity against
the pathogen. Epidemic of a disease is likely to occur when herd immunity
against that disease is very low indicating the presence of a larger number of
susceptible people in the community.
Related Topics