Chapter: Microbiology and Immunology: Immunity
Adaptive (Acquired) Immunity and its Types
Adaptive (Acquired) Immunity
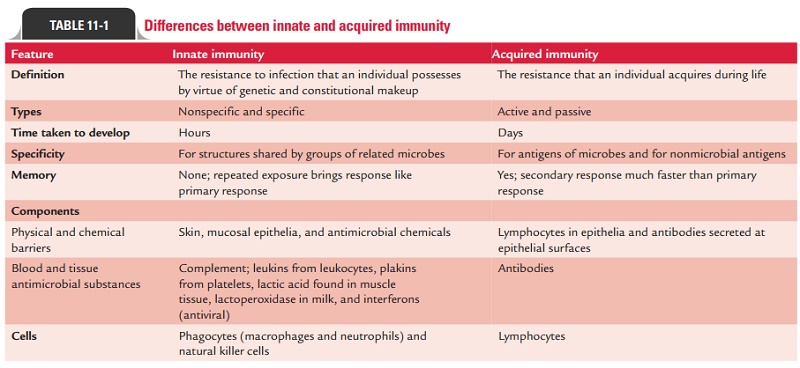
Adaptive immunity is also called acquired immunity, since the potency of immune response is acquired by experience only. Differences between innate and acquired immunity are summarized in Table 11-1.
◗ Types of acquired immunity
Acquired immunity against a microbe may be induced by the host’s response to the microbe or by transfer of antibodies or lymphocytes specific for the microbes. It is of two types: activeimmunity and passive immunity.
Active immunity
The immunity induced by exposure to a foreign antigen is called active immunity. Active immunity is the resistance devel-oped by an individual after contact with foreign antigens, e.g., microorganisms. This contact may be in the form of:
· clinical or subclinical infection,
· immunization with live or killed infectious agents or their antigens, or
· exposure to microbial products, such as toxins and toxoids.
In all these circumstances, the immune system of the host is stimulated to elicit an immune response consisting of antibod-ies and activated helper T (TH) cells and cytotoxic T lympho-cytes/cells (CTLs).
Active immunity develops after a latent period, during which immunity of the host is geared up to act against the microorganism. Hence it is slow in onset, especially during this primary response. However, once the active immunity develops, it is long-lasting and this is the major advantage of the active immunity. The active immunity is of two types: natural active immunity and artificial active immunity.
· Natural active immunity:It is acquired by natural clinicalor subclinical infections. Such natural immunity is long-lasting. For example, individuals suffering from smallpox become immune to second attack of the disease.
· Artificial active immunity: It is induced in individuals byvaccines. There is a wide range of vaccines available against many microbial pathogens. These may be live vaccines, killed vaccines, or vaccines containing bacterial products (Table 11-2).
Mediators of active immunity: Active immunity is mediatedby humoral immunity and cell-mediated immunity. These two types of immunities are mediated by different components of the immune system and function in different ways to kill different types of pathogens.
· Humoral immunity: It is mediated by molecules in theblood and mucosal secretions called antibodies. The anti-bodies are secreted by a subset of lymphocytes known as B cells. The antibodies recognize microbial antigens, combine specifically with the antigens, neutralize the infectivity of microbes, and target microbes for elimina-tion by various effector mechanisms. Humoral immunity is the principal defense mechanism against extracellular microbes.
· Cell-mediated immunity: It is mediated by both activatedTH cells and CTLs. Cytokines secreted by TH cells activate various phagocytic cells, enabling them to phagocytose and kill microorganisms. This type of cell-mediated immune response is especially important against a host of bacte-rial and protozoal pathogens. CTLs play an important role in killing virus-infected cells and tumor cells. They act by killing altered self-cells.
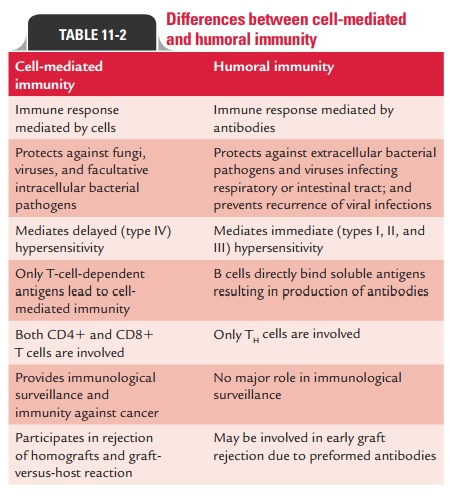
Differences between humoral and cell-mediated immunities are summarized in Table 11-2.
Antigen recognition: Antigens, which are generally very largeand complex, are not recognized in their entirety by lympho-cytes. Instead, both B and T lymphocytes recognize discrete sites on the antigens called antigenic determinants, or epitopes. Epitopes are the immunologically active regions on a com-plex antigen, the regions that actually bind to B-cell or T-cell receptors.
B cells and T cells differ in their mechanisms of antigen recognition. While B cells recognize the antigen by interacting with the epitope on their own, T cells recognize the antigen only when the epitope is “presented” by one of the specialized antigen-presenting cells. Once the antigen has been recognized, these cells then go on to diversify by several intricate mecha-nisms. This diversification helps in conferring the specificity, one of the cardinal characteristics of the immune system.
Major histocompatibility complex (MHC): It is a largegenetic complex with multiple loci. The MHC loci encode two major classes of membrane-bound glycoproteins: class I and class II MHC molecules. Class II molecules present antigens to the TH cells, while class I molecules do the same for CTLs. In order for a foreign protein antigen to be recognized by a T cell, it must be degraded into small antigenic peptides that form complexes with class I or class II MHC molecules. This con-version of proteins into MHC-associated peptide fragments is called antigen processing and presentation.
Passive immunity
When immunity is conferred by transfer of serum or lympho-cytes from a specifically immunized individual, it is known as passive immunity. This is a useful method for conferring resis-tance rapidly, i.e., without waiting for the development of an active immune response. Passive immunity may be natural or artificial.
Natural passive immunity: It is observed when IgG is passedfrom mother to fetus during pregnancy. This forms the basis of prevention of neonatal tetanus in neonates by active immu-nization of pregnant mothers. It is achieved by administering tetanus toxoid to pregnant mothers during the last trimester of pregnancy. This induces production of high level of antibod-ies in mother against tetanus toxin, which are subsequently transmitted from mother to fetus through placenta. The anti-bodies subsequently protect neonates after birth against the risk of tetanus. Natural passive immunity is also observed by passage of IgA from mother to newborn during breast feeding.
Artificial passive immunity: It is induced in an individ-ual by administration of preformed antibodies, generally in the form of antiserum, raised against an infecting agent. Administration of these antisera makes large amounts of antibodies available in the recipient host to neutralize the action of toxins.
The preformed antibodies against rabies and hepatitis A and B viruses, etc. given during incubation period prevent replication of virus, and hence alter the course of infection. Immediate availability of large amount of antibodies is the main advantage of passive immunity. However, short lifes-pan of these antibodies and the possibility of hypersensitiv-ity reaction, if antibodies prepared in other animal species are given to individuals who are hypersensitive to these animal globulins (e.g., serum sickness), are the two noted disadvan-tages of passive immunity.
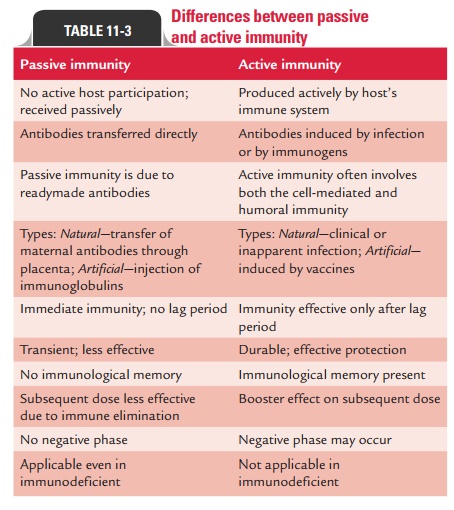
Differences between active and passive immunity are summarized in Table 11-3.
Combined passive–active immunity is carried out by giving both preformed antibodies (antiserum) and a vaccine to provide immediate protection and long-term protection, respectively, against a disease. This approach is followed for prevention of certain infectious conditions, namely, tetanus, rabies, and hepatitis B.
Related Topics