Chapter: Obstetrics and Gynecology: Uterine Leiomyoma and Neoplasia
Treatment of Uterine Leiomyomas
TREATMENT
Most
patients with uterine myomas do not require (surgical or medical) treatment. Treatment
is generally first directedtoward the symptoms caused by the myomas. If this
approach fails (or there are other indications present), sur-gical or other
extirpative procedures may be considered.
For example, if a patient
presents with menstrual aber-rations that are attributable to the myomas, with
bleeding that is not heavy enough to cause her significant hygiene or lifestyle
problems—and the bleeding is also not contribut-ing to iron-deficiency
anemia—reassurance and observation may be all that are necessary. Further
uterine growth may be assessed by repeat pelvic examinations or serial pelvic
ultrasonography.
An attempt may be made to
minimize uterine bleed-ing by using intermittent progestin supplementation and/or prostaglandin synthetase
inhibitors, which decrease the amount of secondary dysmenorrhea and amount of
menstrual flow. If significant endometrial cavity distortion is caused by
intramural or submucous myomas, hormonal supplementation may be ineffective. If
effective, this con-servative approach can potentially be used until the time
of menopause.
Of the surgical options available,
myomectomy is war-ranted in patients
who desire to retain childbearing poten-tial or whose fertility is compromised
by the myomas, creating significant intracavitary distortion. Indications for amyomectomy include a
rapidly enlarging pelvic mass, persistent bleeding, pain or pressure, or
enlargement of an asymptomatic myoma to more than 8 cm in a woman who has not
completed childbearing. Contraindications to myomectomy includepregnancy,
advanced adnexal disease, malignancy, and the situation where enucleation of
the myomas would com-pletely compromise the function of the uterus. Potential
complications of myomectomy include excessive intra-operative blood loss;
postoperative hemorrhage, infection, and pelvic adhesions; and even the need
for emergent hys-terectomy. Within 20 years of a myomectomy procedure, 1 in 4
women has a hysterectomy, the majority for recur-rent leiomyomas.
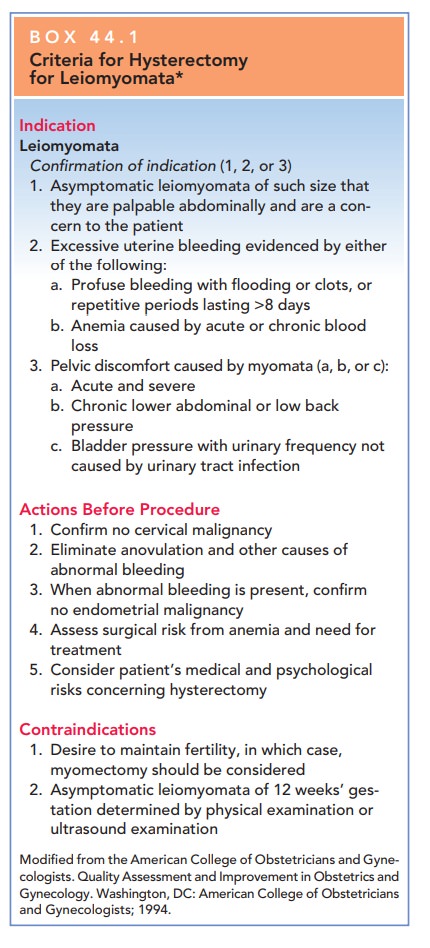
Although hysterectomy is commonly performed for uterine myomas, it should be
considered as definitive treatment only in symptomatic women who have
com-pleted childbearing. Indications should be specific and well-documented
(Box 44.1).
Box 44.1
Criteria for Hysterectomy for Leiomyomata*
Indication
Leiomyomata
Confirmation of indication (1, 2, or 3)
1. Asymptomatic leiomyomata of such size that they are palpable
abdominally and are a con-cern to the patient
2. Excessive uterine bleeding evidenced by either of the following:
a. Profuse bleeding with flooding or clots, or repetitive periods
lasting >8 days
b. Anemia caused by acute or chronic blood loss
3. Pelvic discomfort caused by myomata (a, b, or c):
a. Acute and severe
b. Chronic lower abdominal or low back pressure
c. Bladder pressure with urinary frequency not caused by urinary tract
infection
Actions Before Procedure
·
Confirm
no cervical malignancy
·
Eliminate
anovulation and other causes of abnormal bleeding
·
When
abnormal bleeding is present, confirm no endometrial malignancy
·
Assess
surgical risk from anemia and need for treatment
·
Consider
patient’s medical and psychological risks concerning hysterectomy
Contraindications
·
Desire
to maintain fertility, in which case, myomectomy should be considered
· Asymptomatic leiomyomata of 12 weeks’ ges-tation determined by physical examination or ultrasound examination
Modified from the American College of
Obstetricians and Gyne-cologists. Quality Assessment and Improvement in
Obstetrics and Gynecology. Washington, DC: American College of Obstetricians
and Gynecologists; 1994
Depending on the size of the fibroids and the skill of the
surgeon, both myomec-tomy and hysterectomy can potentially be performed via
laparoscopy. The ultimate decision whether to perform a hysterectomy should
include an assessment of the patient’s future reproductive plans as well as
careful assessment of clinical factors, including the amount and timing of
bleed-ing, the degree of enlargement of the tumors, and the asso-ciated
disability for the individual patient. Uterine myomas alone do not necessarily
warrant hysterectomy.
In addition to surgery,
pharmacologic inhibition of estrogen secretion has been used to treat fibroids.
This is particularly applicable in the perimenopausal years when women are more
likely anovulatory, with relatively more endogenous estrogen. Pharmacologic
removal of the ovar-ian estrogen source can be achieved by suppression of the
hypothalamic-pituitary-ovarian axis through the use of gonadotropin-releasing hormone agonists (GnRHanalogs), which can
reduce fibroid size by as much as 40%to 60%. This treatment is commonly used before a planned hys-terectomy to
reduce blood loss as well as the difficulty of the pro-cedure. It can also be
used as a temporizing medical therapy until natural menopause occurs. Therapy
is generally limitedto 6 months of drug treatment.
In patients with an adequate endogenous
estrogen source, this treatment does not permanently reduce the size of uterine
myomas, as withdrawal of the medication predictably results in regrowth of the
myomas. Although less successful, other pharmacologic agents such as dana-zol have also been used as medical
treatment for myomasby reducing endogenous production of ovarian estrogen.
Other therapeutic modalities have
been introduced, although their efficacy is yet to be demonstrated. Included in
these are myolysis (via direct
procedures or by the deliv-ery of external radio or ultrasonic energy) and
uterine artery embolization (UAE). The safety and efficacy of UAE have been studied to the point that
it is now considered a viable alternative to hysterectomy and myomectomy for
selected patients. The procedure involves selective uterine artery
catheterization with embolization using polyvinyl alcohol particles, which
creates acute infarction of the target myomas. For maximal efficacy, bilateral
uterine artery cannulation and embolization is necessary. In assessing outcomes
data, the three most common symptoms of myomas—bleeding, pressure, and pain—are
ameliorated in over 85% of patients. Acute postembolization pain that requires
hospitalization occurs in approximately 10% to 15% of patients. Other complications
include delayed infection and/or passage of necrotic fibroids through the
cervix up to 30 days after the procedure. UAE
is currently notrecommended as a procedure to consider in patients who desire
future childbearing.MRI-guided focused
ultrasound surgery is a newapproach used to treat myomata. A focused
ultrasound unitdelivers sufficient ultrasound energy to a targeted point to
raise the temperature to approximately 70°C. This results in coagulative
necrosis and a decrease in myoma size. Treatment is associated with minimal
pain and appears to improve self-reported bleeding patterns and quality of
life.
Related Topics