Chapter: Clinical Dermatology: Medical treatment
Topical treatment
Topical
treatment
Percutaneous absorption
A
drug used on the skin must be dissolved or sus-pended in a vehicle (base). The
choice of the drug and of the vehicle are both important and depend on the
diagnosis and the state of the skin. For a drug to be effective topically, it
must pass the barrier to diffusion presented by the horny layer . This requires
the drug to be transferred from its vehicle to the horny layer, from which it
will diffuse through the epidermis into the papillary dermis. Passage through
the horny layer is the rate-limiting step.
The
transfer of a drug from its vehicle to the horny layer depends on its relative
solubility in each (measured as the ‘partition coefficient’). Movement across
the horny layer depends both upon the concentration gradient and on restricting
forces (its ‘diffusion constant’). In general, non-polar substances penetrate
more rapidly than polar ones. A rise in skin temperature and in hydration, both
achieved by covering a treated area with polyethylene occlusion, encourages
penetration.
Some
areas of skin present less of a barrier than do others. Two extreme examples
are palmar skin, with its impermeable thick horny layer, and scrotal skin,
which is thin and highly permeable. The skin of the face is more permeable than
the skin of the body. Body fold skin is more permeable than nearby unoc-cluded
skin. In humans, absorption through the hair follicles and sweat ducts is of
little significance and the amount of hair on the treated site is no guide to
its permeability.
In
many skin diseases, the horny layer becomes abnormal and loses some of its
barrier function. The abnormal nucleated (parakeratotic) horny layers of
psoriasis and chronic eczema, although thicker than normal, have lost much of
their protective qualities. Water loss is increased and therapeutic agents
penet-rate more readily. Similarly, breakdown of the horny layer by chemicals
(e.g. soaps and detergents) and by physical injury will allow drugs to
penetrate more easily.
In
summary, the penetration of a drug through the skin depends on the following
factors:
•
its concentration;
•
the base;
•
its partition coefficient;
•
its diffusion constant;
•
the thickness of the horny layer;
•
the state, including hydration, of
the horny layer; and
•
temperature.
Active ingredients
These
include corticosteroids, tar, dithranol, anti-biotics, antifungal and antiviral
agents, benzoyl per-oxide, retinoic acid and many others. The choice depends on
the action required, and prescribers should know how each works. As topical
steroids are the mainstay of much local derma-tological therapy, their
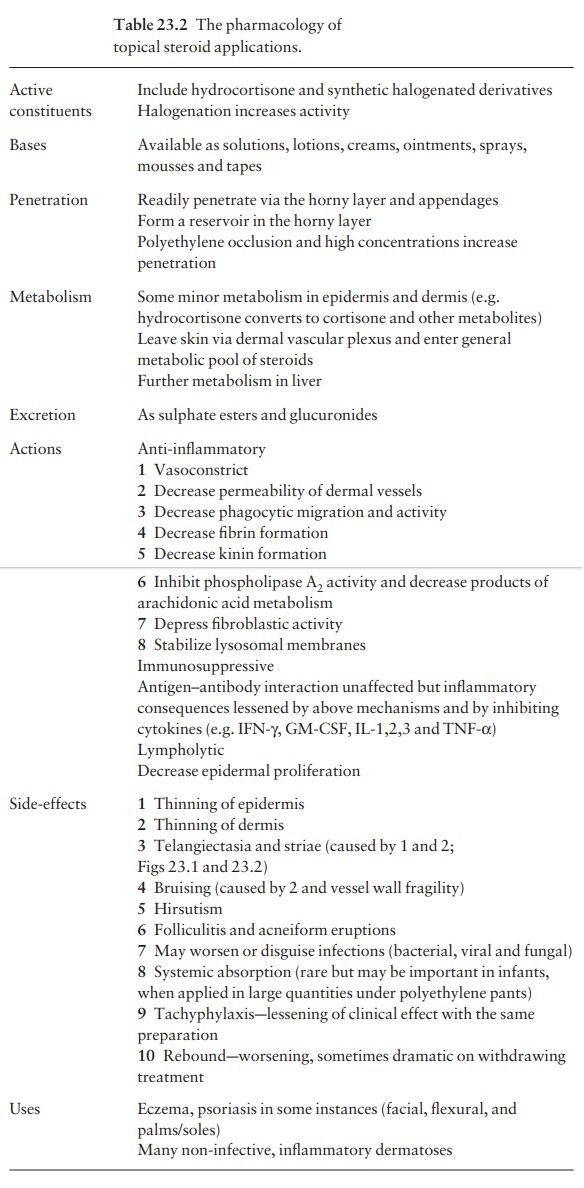
pharmacology is summarized in Table 23.2.
Vehicles (bases)
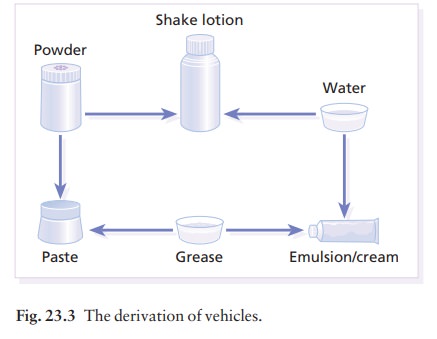
Most
vehicles are a mixture of powders, water and greases (usually obtained from
petroleum). Figure 23.3 shows that blending these bases together produces
preparations that retain the characteristics of each of their components.

A
vehicle should maximize the delivery of top-ical drugs but may also have useful
properties in its own right. Used carelessly, vehicles may even do harm.
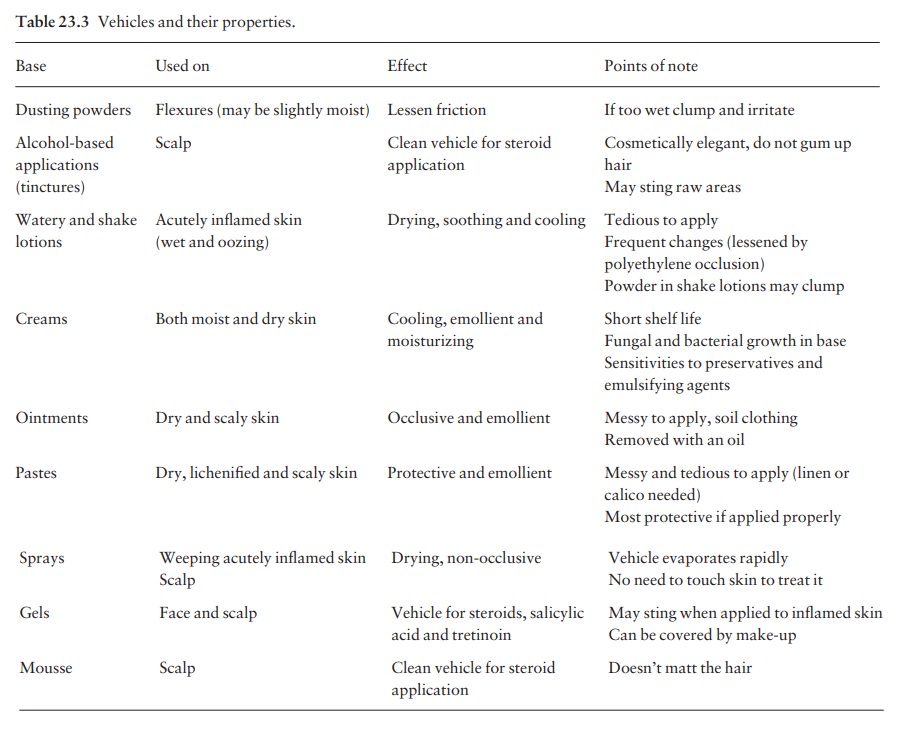
Suggested indications are shown in Table 23.3. The choice of vehicle depends
upon the action desired, availability, messiness, ease of application and cost.
Individual vehicles
Dusting
powders are used in the folds to lessen fric-tion between opposing surfaces.
They may repel water (e.g. talc) or absorb it (e.g. starch); zinc oxide powder
has an absorptive power midway between these extremes. Powders ought not be
used in moist areas where they tend to cake and abrade.
Watery
lotions evaporate and cool inflamed areas. This effect is hastened by adding an
alcohol, but glyc-erol or arachis oil slow evaporation and retain skin
moisture. Substances that precipitate protein (astrin-gents; e.g. silver
nitrate) lessen exudation.
Shake
lotions are watery lotions to which powder has been added so that the area for
evaporation is increased. These lotions dry wet weeping skin. When water has
evaporated from the skin, the powder particles clump together and may become
abrasive. This is less likely if an oil such as glycerol has been added.
Creams are used for their cooling, moisturizing and emollient effects. They are either oil-in-water emulsions [e.g. aqueous cream (UK), acid mantle cream (USA)] or water-in-oil emulsions [e.g. oily cream (UK), cold cream (USA)]. Emulsifying agents are added to in-crease the surface area of the dispersed phase and that of any therapeutic agent in it.
Ointments
are used for their occlusive and emol-lient properties. They allow the skin to
remain supple by preventing the evaporation of water from the horny layer.
There are three main types:
1 those
that are water-soluble (macrogols, polyethy-lene glycols);
2
those that emulsify with water; and
3 those that
repel water (mineral oils, and animal andvegetable fats).
Pastes
are used for their protective and emollient properties and usually are made of
powder added to a mineral oil or grease. The powder lessens the oil’s occlusive
effect.
Variations
on these themes have led to the numer-ous topical preparations available today.
Rather thanuse them all, and risk confusion, doctors should limit their choice
to one or two from each category. Table 23.3 summarizes the properties and uses
of some common preparations.
Preservatives
Water-in-oil
emulsions, such as ointments, require no preservatives. However, many creams
are oil-in-water emulsions that permit contaminating organ-isms to spread in a
continuous watery phase. These preparations therefore, as well as lotions and
gels, require the incorporation of preservatives. Those in common use include
the parahydroxybenzoic acid esters (parabens), chlorocresol, sorbic acid and
propy-lene glycol. Some puzzling reactions to topical pre-parations are based
on allergy to the preservatives they contain
Methods of application
Ointments
and creams are usually applied sparingly twice daily, but the frequency of
their application will depend on many factors including the nature, severity
and duration of the rash, the sites involved, conveni-ence, the preparation
(some new local steroids need only be applied once daily; Formulary 1) and,
most important, on common sense. In extensive erup-tions, a tubular gauze cover
keeps clothes clean and hampers scratching (see Fig. 7.19).
Three
techniques of application are more special-ized: immersion therapy by bathing,
wet dressings (compresses) and occlusive therapy.
Bathing
Once-daily
bathing helps to remove crusts, scales and medications. After soaking for about
10 min, the skin should be rubbed gently with a sponge, flannel or soft cloth;
cleaning may be made easier by soaps, oils or colloidal oatmeal.
Medicated
baths are occasionally helpful, the most common ingredients added to the bath
water being bath oils, antiseptics and solutions of coal tar.
After
cleaning, the most important function of a bath is hydration. The skin absorbs
water and this can be held in the skin for some time if an occlusive oint-ment
is applied after bathing.
Older
patients may need help to get into a bath and should be warned about falling if
the bath contains an oil or another slippery substance.
Wet dressings (compresses)
These
are used to clean the skin or to deliver a topical medication. They are
especially helpful for weeping, crusting and purulent conditions such as
eczema,. Five or six layers of soft cloth (e.g. cotton gauze) are soaked in the
solution to be used; this may be tap water, saline, an astringent or antiseptic
solution, and the compress is then applied to the skin. Open dressings allow
the water to evaporate and the skin to cool. They should be changed frequently,
e.g. every 15 min for 1 h.
Closed dressings are covered with a plastic (usually polyethylene) sheet; they do not dry out so quickly and are usually changed twice daily. They are especially helpful for debriding adherent crusts and for draining exudative and purulent ulcers.
Occlusive therapy
Sometimes
steroid-sensitive dermatoses will respond to a steroid only when it is applied
under a plastic sheet to encourage penetration. This technique is best reserved
for the short-term treatment of stubborn localized rashes. The drawback of this
treatment is that the side-effects of topical steroid treatment (Table 23.2)
are highly likely to occur. The most important is systemic absorption if a
large surface area of skin, relative to body weight, is treated (e.g. when
steroids are applied under the polyethylene pants of infants).
Monitoring local treatment
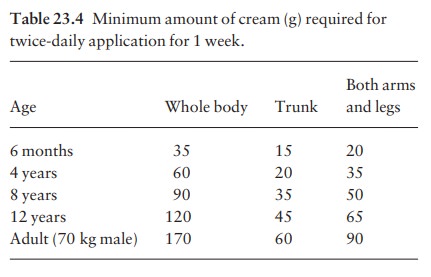
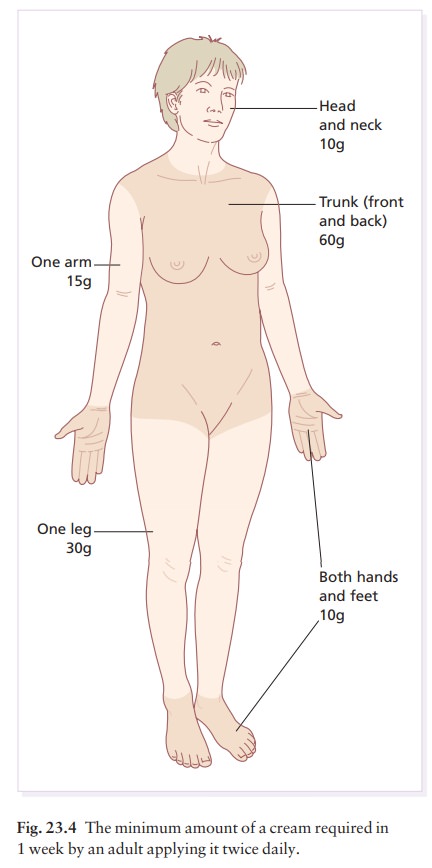
One
common fault is to underestimate the amount required. The guidelines given in
Table 23.4 and Fig. 23.4 are based on twice daily applications. Lotions go
further than creams, which go further than oint-ments and pastes.
Pump dispensers have recently become available for some topical steroids which allow measured amounts to be applied. Alternatively, ‘fingertip units’ (Fig. 23.5) can increase the accuracy of prescribing. As a guide, You know how much digoxin your patients are taking, but do you know how much of a topical corticosteroid they are applying? Keep a check on this.
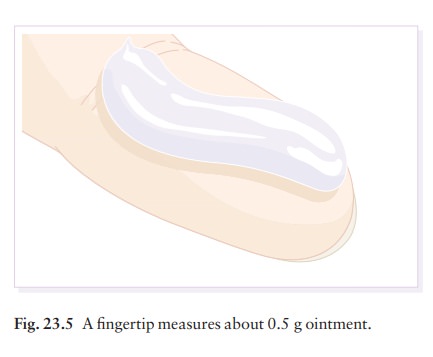
one
fingertip unit in an adult male from a standard nozzle provides 0.5 g ointment.
Related Topics