Chapter: Pathology: Endocrine Pathology
Thyroid Gland - Pathology
THYROID GLAND
Multinodular goiter (nontoxic goiter) refers to
an enlarged thyroid gland with mul-tiple colloid nodules. Females are affected
more often than males. It is frequently asymptomatic, and the patient is
typically euthyroid, with normal T4, T3, and TSH. Plummer
syndrome is the development of hyperthyroidism (toxic multinodular goi-ter)
late in the course.
Microscopically, the tissue
shows nodules of varying sizes composed of colloid folli-cles. Calcification,
hemorrhage, cystic degeneration, and fibrosis can also be present.
Hyperthyroidism
The term hyperthyroidism is used when the mean
metabolic rate of all cells is increased due to increased T4 or T3. Clinical
features include tachycardia and pal-pitations; nervousness and diaphoresis;
heat intolerance; weakness and tremors; diarrhea; and weight loss despite a
good appetite. Lab studies show elevated free T4.
•
In primary hyperthyroidism, TSH is decreased.
•
In secondary and tertiary hyperthyroidism, TSH is elevated.
Graves disease is an autoimmune disease
characterized by production of IgG auto-antibodies to the TSH receptor. Females
are affected more frequently than males, with peak age 20–40. Clinical features
include hyperthyroidism, diffuse goiter, oph-thalmopathy (exophthalmus), and
dermopathy (pretibial myxedema). Microscopi-cally, the thyroid has hyperplastic
follicles with scalloped colloid.
Other causes of hyperthyroidism include toxic multinodular goiter, toxic
adenoma (functioning adenoma
producing thyroid hormone), and Hashimoto and subacute thyroiditis (transient
hyperthyroidism).
Hypothyroidism
The term hypothyroidism is used when the mean
metabolic rate of all cells is decreased due to decreased T4 or T3. Clinical
features include fatigue and lethargy; sensitivity to cold temperatures;
decreased cardiac output; myxedema (accumulation of proteoglycans and water);
facial and periorbital edema; peripheral edema of the hands and feet; deep
voice; macroglossia; constipation; and anovulatory cycles. Lab studies show
decreased free T4.
•
In primary hypothyroidism, TSH is elevated.
•
In secondary and tertiary hypothyroidism, TSH is decreased.
Iatrogenic hypothyroidism is the most common cause of
hypothyroidism in the United States, and is
secondary to thyroidectomy or radioactive iodine treatment. Treatment is
thyroid hormone replacement.
Congenital hypothyroidism (cretinism) in endemic
regions is due to iodine defi-ciency during intrauterine and neonatal life, and
in nonendemic regions is due to thyroid dysgenesis. Patients present with
failure to thrive, stunted bone growth and dwarfism, spasticity and motor
incoordination, and mental retardation. Goiter is seen in endemic cretinism.
Endemic goiter is due to dietary deficiency
of iodine; it is uncommon in the United States.
Thyroiditis
Hashimoto thyroiditis is a chronic autoimmune
disease characterized by immune destruction of the thyroid
gland and hypothyroidism. It is the most common noni-atrogenic/nonidiopathic
cause of hypothyroidism in the United States; it most com-monly causes painless
goiter in females more than males, with peak age 40–65.
Hashimoto thyroiditis is the
most common cause of hypothyroidism (due to destruction of thyroid tissue),
though the initial inflammation may cause transient hyperthyroidism
(hashitoxicosis). Hashimoto may be associated with other autoim-mune diseases
(SLE, rheumatoid arthritis, Sjögren syndrome, etc.), and it has an increased
risk of non-Hodgkin B-cell lymphoma. Grossly, Hashimoto produces a pale,
enlarged thyroid gland; microscopically, it shows lymphocytic inflammation with
germinal centers and epithelial “Hürthle cell” changes.
Subacute thyroiditis (also called de Quervain
thyroiditis and granulomatous thy-roiditis) is the second most common form of
thyroiditis; it affects females more than males, with peak age 30–50. Patients
may complain of odynophagia (pain on swallowing).
•
Typically preceded by a viral illness
•
Produces a tender, firm, enlarged thyroid gland
•
May be accompanied by transient hyperthyroidism
Microscopy shows
granulomatous thyroiditis. The disease typically follows a self-limited course.
Riedel thyroiditis is a rare disease of unknown
etiology, characterized by destruc-tion of the thyroid gland by dense fibrosis
and fibrosis of surrounding structures (trachea and esophagus). It affects
females more than males, and most patients are middle-aged.
•
Causes an irregular, hard thyroid that is adherent to adjacent
structures
•
May clinically mimic carcinoma and present with stridor, dyspnea,
or dysphagia
Microscopic exam shows dense
fibrous replacement of the thyroid gland with chronic inflammation. Reidel
thyroiditis is associated with retroperitoneal and mediastinal fibrosis.
Thyroid Neoplasia
Thyroglossal duct cyst presents as a midline neck
mass in a young patient. Its epi-thelium varies with location (squamous/respiratory).
It may become infected and painful. Treatment is surgical.
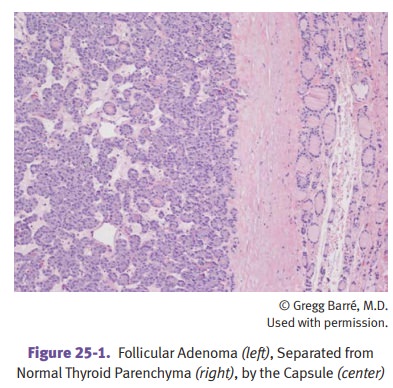
Adenomas: follicular adenoma is the most common.
Clinically, adenomas are usu-ally painless, solitary, encapsulated nodules that
appear “cold” on thyroid scans. They may be functional and cause
hyperthyroidism (toxic adenoma).
Papillary carcinoma accounts for 80% of malignant
thyroid tumors. It affects females more than males, with peak
age 20–50. Radiation exposure is a risk factor. Resection is curative in most
cases. Radiotherapy with iodine 131 is effective for metastases. The prognosis
is excellent, with 20-year survival 90% due to slow growth and metastasis to
regional cervical lymph nodes. There are chromosomal rearrangements of the RET oncogene.
Microscopically, the tumor
typically exhibits a papillary pattern. Occasional psam-moma bodies may be
seen. Characteristic nuclear features include clear “Orphan Annie eye” nuclei,
nuclear grooves, and intranuclear cytoplasmic inclusions. Lym-phatic spread to
cervical nodes is common.
Follicular carcinoma accounts for 15% of malignant
thyroid tumors. It affects females more than males, with peak
age 40–60. Hematogenous metastasis to the bones or lungs is common. These
cancers are microscopically distinguished from follicular adenoma by the
presence of capsular invasion.
Medullary carcinoma accounts for 5% of malignant
thyroid tumors. It arises from C cells (parafollicular cells)
and secretes calcitonin. Microscopic exam shows nests of polygonal cells in an
amyloid stroma. A minority of cases (25%) is associated with MEN 2 and MEN 3
syndromes, and those cases tend to be multicentric. Activating RET mutations are present in familial
and sporadic types.
Anaplastic carcinoma affects females more than
males, with peak age >60. It can present with a firm,
enlarging, and bulky mass, or with dyspnea and dysphagia. The tumor has a
tendency for early widespread metastasis and invasion of the tra-chea and
esophagus. Microscopically, the tumor is composed of undifferentiated,
anaplastic, and pleomorphic cells. This very aggressive tumor is often rapidly
fatal.
Related Topics