Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Thermoregulation, Hypothermia, & Malignant Hyperthermia
Thermoregulation & Hypothermia
THERMOREGULATION
& HYPOTHERMIA
Hypothermia,
usually definedasabody tempera-ture less than
36°C, occurs frequently
during anes-thesia and surgery. Unintentional perioperative hypothermia is more
common in patients at the extremes of age, and in those undergoing abdominal
surgery or procedures of long duration, especially with cold ambient operating
room temperatures; it will occur in nearly every such patient unless steps are
taken to prevent this complication.
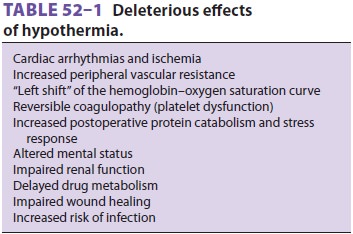
Hypothermia reduces metabolic oxygen requirements and can be protective
during cere-bral or cardiac ischemia. Nevertheless, hypother-mia has multiple deleterious physiological effects (Table 52–1). Infact,
unintendedperioperativehypothermia has been associated with an increased
mortality rate.
Core temperature is normally the same as the
central venous blood temperature (except during periods of relatively rapid
temperature change as can occur during extracorporeal perfusion). When there is
no attempt to actively warm an anesthetized patient, core temperature usually
decreases 1–2C during the first hour of general anesthesia (phase one), followed
by a more gradual decline during the ensuing 3–4 h (phase two), eventually
reaching a point of steady state (phase three). With general, epidural, or
spinal anesthesia redistribution of heat from warm “central” compartments (eg,
abdomen, thorax) to cooler peripheral tissues (eg, arms, legs) from
anesthetic-induced vasodilation explains most of the initial decrease in
temperature
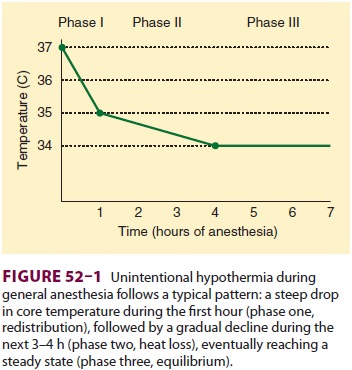
during phase one, with actual heat loss from
the patient to the environment being a minor contribu-tor. Continuous heat loss
to the environment appears to be primarily responsible for the slower
subse-quent decline during phase two. At steady state, heat loss equals
metabolic heat production (Figure 52–1).In the normal unanesthetized patient
the hypothalamus maintains core body temperature within very narrow tolerances,
termed the interthreshold range, with the threshold for sweating and
vasodilation at one extreme and the threshold for vasoconstriction and
shivering at the other. Increasing core temperature a fraction of a degree
induces sweating and vasodilation, whereas a mini-mally reduced core
temperature triggers vasoconstriction and shivering. Anesthetic agents inhibit
central thermoregulation by interfering with these hypothalamic reflex
responses. For example, isoflurane produces a dose-dependent decrease in the
threshold temperature that triggers vasoconstriction (3C decrease for each
percent of inhaled isoflurane). Both general and regional anesthetics increase
the interthreshold range, albeit by different mechanisms. Spinal and epidural
anes-thetics, like general anesthetics, lead to hypothermia by causing
vasodilation and internal redistribu-tion of heat. The accompanying thermoregulatory
impairment from regional anesthetics that allows continued heat loss is
likely due to altered percep-tion by the hypothalamus of temperature in the
anesthetized dermatomes rather than a central drug effect, as with general
anesthetics.
Intraoperative Considerations
A cold ambient temperature in the operating
room, prolonged exposure of a large wound, and the use of large amounts of
room-temperature intravenous fluids or high flows of unhumidified gases can
con-tribute to hypothermia. Prewarming the patient
forhalf an hour with convective forced-air warming
blankets prevents phase one
hypothermia by elim-inating the central–peripheral temperature gradi-ent. Methods tominimizephase twohypothermiafrom heat loss during anesthesia
include use of forced-air warming blankets and warm-water blan-kets, heated
humidification of inspired gases, warm-ing of intravenous fluids, and
increasing ambient operating room temperature. Passive insulators such as
heated cotton blankets or so-called space blankets have limited utility unless
virtually the entire body is covered.
Postoperative Considerations
Shivering can occur in postanesthesia care
units (PACUs) or critical care units as a result of actual hypothermia or
neurological aftereffects of general anesthetic agents. Shivering is also
common imme-diately postpartum. Shivering in such instances rep-resents the
body’s effort to increase heat production and raise body temperature and may be
associated with intense vasoconstriction. Emergence from even brief general anesthesia
is sometimes also associated with shivering. Although the shivering can be part
of nonspecific neurological signs (posturing, clonus, or the Babinski sign)
that are sometimes observed during emergence, shivering is most often
associ-ated with hypothermia and volatile anesthetics. Regardless of the
mechanism, shivering appears to be more common after longer durations of
surgery and the use of greater concentrations of a volatile agent. Occasionally
it is intense enough to cause hyperthermia (38–39°C) and metabolic acidosis, both of which
promptly resolve when the shivering stops. Both spinal and epidural anesthesia
lower th shivering threshold and vasoconstrictive response to hypothermia;
shivering may also be encountered in the PACU following regional anesthesia.
Other causes of shivering should be excluded, such as sep-sis, drug allergy, or
a transfusion reaction. Intense shivering may increase oxygen consumption, CO2 production, and cardiac output. These
physiologi-cal effects are often poorly tolerated by patients with preexisting
cardiac or pulmonary impairment.
Postoperative shivering may increase oxygen consumption as much as
fivefold, may decrease arte-rial oxygen saturation, and may be associated with
an increased risk of myocardial ischemia. Although postoperative shivering can
be effectively treated with small intravenous doses of meperidine (12.5– 25 mg)
in adults, the better option is to reduce the likelihood of shivering by
maintaining normother-mia. Shivering in intubated and mechanically venti-lated
patients can also be controlled with sedation and a muscle relaxant until
normothermia is rees-tablished and the effects of anesthesia have dissipated.
Postoperative hypothermia should be treated
with a forced-air warming device, if available;alternately
(but less satisfactorily) warming lights or heating blankets can be used to
restore body temper-ature to normal. Hypothermia has been associated with an
increased incidence of myocardial ischemia, arrhythmias, increased transfusion
requirements, and increased duration of muscle relaxant effects, the latter of
which can be especially harmful in the recently extubated patient.
Related Topics