Chapter: Forensic Medicine: Introduction
The inquest
The inquest
The Inquests Act provides, inter alia, for
``holding of inquests in cases of deaths or alleged deaths apparently occurring
from other than natural causes, and for matters incidental thereto ...''
How does the inquest court come to know of an alleged non-natural death?
Where a medical practitioner is unable to
certify that the death of his patient (or other person) was solely and
exclusively due to natural causes, he isThis section is based on Smith (1986)
and Strauss (1991:424).required to inform a policeman accordingly. In such
cases the doctor does not issue a death certificate. The police will inform a
magistrate accordingly, who will request the police to investigate the matter.
The police will then report to the public prosecutor.
The Act reads:
Any person [this includes the doctor or nurse]
who has reason to believe that ... a person has died ... due to other than
natural causes shall report accordingly to a policeman, unless he has reason to
believe that a report has or will be made by any other person.
Any policeman who has reason to believe that any
person had died ... from other than a natural cause shall investigate the
circumstances of the death or alleged death.
How does the medical practitioner become involved in the medical investigation of death?
The magistrate to whom the death is reported
must, if he deems it expedient in the interests of justice, cause it to be
examined by a medical practitioner (eg a forensic pathologist) ``who may, if he
deems it necessary for the purpose of ascertaining with greater certainty the cause
of death make or cause to be made an examination of any internal organ, or any
part or any contents of the body, or any other substance or thing''. For the
purpose of this examination ``any part or internal organ or contents of a body
may be removed'' and ``removed to any place''.
If the pathologist or any medical practitioner
has been involved in the treatment of the deceased before death, it is the
policy of the Department of Health that he should advise the magistrate
accordingly so that he can seek the assistance of another pathologist or
medical practitioner in order to conduct the post-mortem examination. In
practice he will generally consult with the forensic consultant, in other words
the chief pathologist for the region.
The post-mortem examination
The extent and nature of the post-mortem
examination is not prescribed by statute, but the medical practitioner
undertaking this task would be well advised to follow with discretion the
procedure as laid out in the report form provided for this purpose.
Who may be present at the post-mortem examination?
A police officer or another medical practitioner
nominated by any person, who satisfies the magistrate that he has a
``substantial and peculiar interest in the issue of the examination may be
present at the post-mortem examination, as well as any other person permitted
by the magistrate or the medical practitioner conducting the post-mortem
examination''. The attendance of students is included in the latter provision.
The doctor performing the autopsy should welcome the presence of a colleague,
who may be appointed by the relatives to represent their interests, as he
should have nothing to hide, and a second opinion is generally helpful (Strauss
1991:424).
Report of the examination
The findings at an autopsy, which are recorded
as the autopsy is done, are generally later transcribed on the prescribed form,
with (it is hoped) meticulous attention to relevant factual detail and
accuracy; these findings represent the personal factual observations of the medical
practitioner performing the examination (Nel 1986:5).
Subsequent proceedings and findings
The report is submitted to the investigating
police officer in the form of an affidavit. Together with the other relevant
documents it is submitted to the public prosecutor, who may call for additional
information. If criminal proceedings are not instituted, the prosecutor will
submit the documents and other information to the magistrate.
In terms of the Inquests Act the judicial
officer shall record a finding on the following:
·
the identity of the deceased
·
the date or likely date of death
·
the cause or likely cause of death
·
whether the death was brought about by any act or omission involving or
amounting prima facie to an offence on the part of any person
If the judicial officer is unable to record any
such finding she shall record that fact. It should be appreciated that the
evidence which justifies a finding of a likely cause of death may not stand the
test of a criminal trial or a civil action.
Both competent medical acts and omissions may
result in a death (eg death during a heart transplant operation or following
failure to institute specific treatment in a case of cerebral haemorrhage), but
such an act or omission need not constitute an offence in the sense of criminal
negligence.
If the body has been destroyed (eg by cremation)
or if no body can be recovered (eg in a sea disaster) and if the evidence
proves beyond reasonable doubt that the person has died, the judicial officer
shall accordingly record a finding of death and then proceed to make a finding
as in the case of all inquests.
At the termination of the inquest the judicial
officer is required to submit the record to the Director of Public Prosecution
in the following circumstances:
·
if she cannot make a finding
·
if she makes a finding that death was brought about by an act or
omission involving or amounting to an offence
·
if the Director of Public Prosecutions has requested that this be done
The Director of Public Prosecutions has the
powers to re-open an inquest or to permit exhumation of a body for further
investigation.
How do the findings affect the medical practitioner?
Trust not the physician
His antidotes are poison,
and he slays more than you rob.
(Shakespeare: Timon of Athens)
One may often have heard the above. However ...
``we cannot freely and wisely choose the right way for ourselves unless we know
both good and evil'' (Helen Keller).
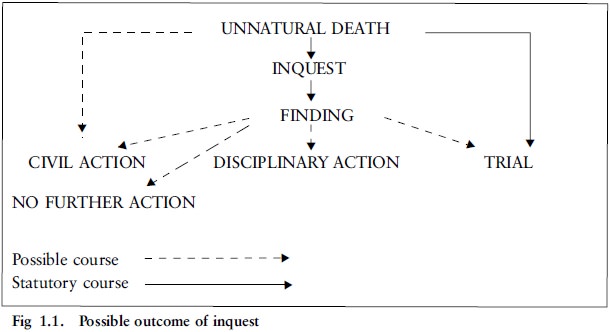
If the finding in any way reflects adversely on
a medical practitioner, criminal and/or civil action or a disciplinary inquiry
by the Health Professions Council of South Africa may ensue (fig 1.1).
An inquest can often help to identify the
medical ``good and evil'' because not infrequently it has a major medical component
which may reveal or conversely justify apparent medical shortcomings, and so
play an important role as an external audit of the quality of medical care.
Consequently the events leading up to inquests, the evidence and procedure, the
findings and the possible consequences arising from the findings should be of
interest to medical practice in its broadest sense, and should not be
restricted only to the forensic medical practitioner.
It is important that people develop a knowledge
of and interest in medical jurisprudence, particularly in the light of the
disturbing world-wide trends towards litigation against doctors and hospitals,
and also because patients are (rightly so) becoming more aware of what can
legitimately be expected as ``reasonably competent'' attention in the various
categories of medical medicine.
General reasons for censure of the medical practitioner at an inquest
The major cause for censure of the medical
practitioner can be summed up in the words ``failure to ...''. This may either
be the failure to institute acceptable treatment of the patient, or failure to
adhere to ethical norms.
The following questions need to be asked by the
doctor preparing to give evidence on a particular form of treatment:
·
Was the drug or procedure the correct choice, and was I competent to
administer it?
·
Was there a clear indication for its use?
·
Was I aware of dangers involved and contra-indications?
·
Did I attempt to anticipate by generally acceptable methods the
possibility that the patient might exhibit any idiosyncrasy to such use
·
Was I in a position to skilfully apply the necessary counteractants?
·
Was I in a position to skilfully manage any complications due to
intervention?
Related Topics