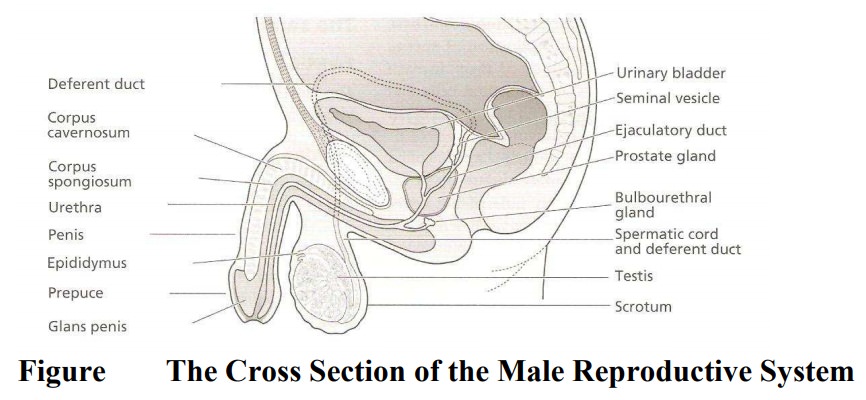
Chapter: Maternal and Child Health Nursing : The Male Reproductive System
The Male Reproductive System
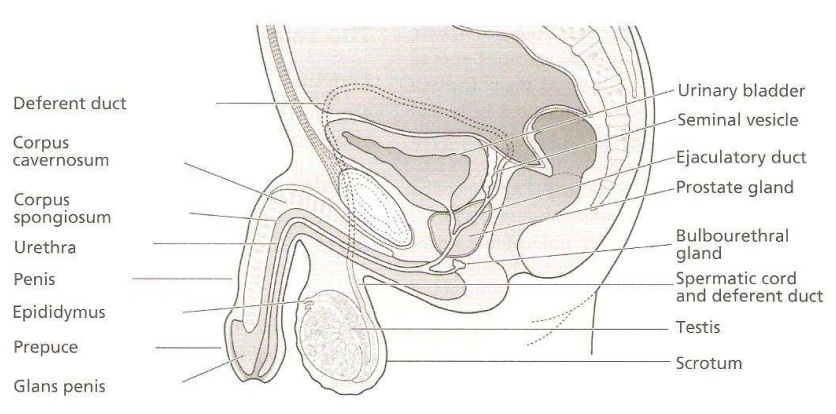
The Male Reproductive System
The male
reproductive system is made up two main parts.
1.
The External
2.
The internal parts
The External Organs
1. The Penis
It has
its root in the perineum with the lower 2/3rd of the body suspended outside in
front of the scrotal sac. It is made up of three bundles of spong-like
erectitle tissues:
1.
2 the corporal cavernosa on the lateral columns in
front of the urethra
2.
The corpus spongiosum on the posterior column which
contains the urethra enclosed in a firm sheath of firm tissue with rich blood
supply and covered with the skin. The skin continues with the scrotum and the
groins. The skin double fold backwards on itself at the glans penis to form the
prepuce (foreskin) which is usually removed during circumcision. The penis
transmites a portion of the urethra which acts as a passage for semen as well
as excretion of urine… During sexual excitement the pe nis becomes larger,
rounder, firmer and erect to be able to penetrate and deposit semen near the
cervix. Stimulation of the nervous system increases blood supply to the organ.
This
erections tart at puberty and may result in wet dream in adolescent boy. There
is a small sphincter in the urethra which prevent semen from entering the
bladder and urine from the urethra mixing with the semen during intercourse.
2. The Scrotum
It is a
sensitive pouch-like sac covered with wrinkled skin and hair from which the
penis hangs. It lies in front of the thighs, behind the penis and is thickly
pigmented. The scrotum is divided by a fibrous septum called Dartos muscle into
two cavities each of which contain a testis epididymis and initial portion of
the vas deference. The muscles contract in cold weather and relax in hot
weather to ensure normal temperature around the testes. Next to the clartos
muscle lies the cremaster muscle and fascia. It protects the testes from
injuries.
The Internal Organs
1. The Testes
The
testes are the male reproductive glands (Gonads), equivalent to the female
ovaries. They are formed in the fetal abdomen at the lumber region just below
the kidneys at about 28th week of gestation. The testes descend into
the scrotum via the right and left inguinal canal, toward the end of pregnancy.
They are suspended by spermatic ducts. The testis is ovoid in shape & white
in colour.
Size: 4-4.5cm long, 2.5cm wide 3cm
thick and 10-14gm ormore in weight, depending on the heftiness of the individual
man structure. Each testis is surrounded by 3 coverings of glandula tissue.
1.
Tunica
Vaginalis: This is the thick outer covering and is adouble
fold of a down growth of the abdominal and pelvic peritoneum brought down with
the descending testis when it descends. The visceral layer surrounds the testes
while the parietal lines the Germaters muscle.
2.
Tunica
Albuginea: This is a fibrous tissue coat surroundingthe testes
under the vaginalis. Ingrowths of albuginea form septa dividing the glandular
tissue into 200-400 lobules. Each contains convulated seminiferous tubules
lined with germinal epithelium which produce sperm (Spermatogenesis) from
puberty. Surrounding the tabula are connective tissue stroma which contains
cluders dendox cells (Leydig cells) cells which secrete testosterone.
3.
Tunica
Vasculosa: This consists of network of capillariessupported by
delicate connective tissues. They surround each lobule of the testes. The
testes must be kept below body temperature in order to function properly, hence
they are situated outside the body. Inflammation of the testis is known as Ochitis.
Cryptorchidism: Complete failure of the testes to
descend into thescrotum. Such testes are destroyed due to high body
temperature.
2. The Epididymis
This is a
fine convoluted tubule about 6 metre in length connecting the testis and the
vas defense. It is found at the posterior aspect of the testis. It produces
substance which stimulates the development of the sperm. The sperms are stored
here to become mature and motile
3. Vas Deferens
A
continuation of the epididymis, commences at the tail and, passes upwards
behind the testis through the inguinal canal and ascends medially towards the
posterior wall of the bladder; enter the pelvic cavity where it connects with
the seminal duct. These are the tubes ligated during vasectomy; it is about
450cmlong. The vas deferens duct is surrounded by smooth muscle the peristaltic
contraction of the smooth muscle tissue help propel sperm cells through the
duct.
4. Seminal Vesicles
These are
small irregular Pyramid shaped sacs lying between the base of the bladder and
the rectum. They are about 5cm long. They are composed of columnar epithelium,
muscle and fibrous tissues. They secrete yellowish fluids which is an essential
component of seminal fluid. Each vesicle opens into the seminal duct which
joins the vas deferens on the corresponding side of the ejaculatory duct. The
fluid contains fructose and other nutrients to nourish the sperm. Forms
nutrients to nourish the sperm constitute about 60% of the semen and give it
its co lour.
5. Ejaculatory Ducts
They are
two small muscular ducts about 2cm long. Pass through the prostate gland and
connects with the vas deferens and opens into the urethra. They carry the
spermatozoa and seminal fluid to the urethra.
6. Prostate Gland
Is a cone
shaped structure, about the size of a walnut.4cm long, 3cm wide, 2cm deep and
8g in weight. It lies below the bladder, surrounding the upper part of the
urethra in direct contact with the neck of bladder. It is composed of glandular
tissue and involuntary (Columnar epithelium) muscle enclosed in fibrous
capsule. It secretes alkaline fluid which makes up 30% of semen. It is added to
the sperm, and the muscle fiber aids ejaculation of the sperm. The fluid neutralizes
the acidity of the vagina during intercourse. It gives the characteristic
odour. Enlargement of prostate gland in old men causes urine retention.
7. Cowper’s Glands (Bulbo Urethral
Glands)
They are
two small glands about the size of a cowpea, yellow in colour and lie below the
prostate gland. The ducts about 3cm long open into the urethra before reaching
the penile portion. The secretion is alkaline in nature and is added to the
seminal fluids and also help to lubricate the penis during sexual activities.
8. The Urethra
Is a
tube, about 8 cm long, travels from the bladder to the tip of the penis. Urine
passes through it as well as a passage for semen during sexual intercourse. The
muscle at the neck of the bladder closes it up to prevent semen from entering
the bladder during sexual intercourse.
Related Topics