Histoplasmosis, Pathogenesis and Pathology, Clinical Features, Laboratory Diagnosis | Medical Mycology - Systemic Mycoses | 12th Microbiology : Chapter 9 : Medical Mycology
Chapter: 12th Microbiology : Chapter 9 : Medical Mycology
Systemic Mycoses
Opportunistic Mycoses
The
opportunistic systemic mycoses are infections found in patients with underlying
pre disposing conditions. It is produced by non pathogenic or contaminant fungi
in a host, where the immunological defense mechanisms are weakened by
endogenous causes like cancer, leukemia or exogenous causes like immunosuppressive
therapy and AIDS. The examples of opportunistic mycoses are Candidiasis,
Cryptococcosis, Aspergillosis and zygomycosis.
Candidiasis
Candidiasis
is the commonest fungal disease found in humans affecting mucosa, skin, nails and
internal organs of the body. It
is caused by yeast like fungi called Candida
albicans . The infection may be acute
or chronic, superficial or deep and found mainly as secondary infection in
individuals with immune compromised condition.
The fungus candida albicans is response ble for most vaginal yeast infections. Your vagina naturally contains a
balancedmix of yeast, including candida, and bacteria. Certain bacteria
(lactoba-cillus) act to prevent an overgrowth
of yeast. But that balance can be disrupted.
Pathogenesis and Pathology
Some of
the virulence factors contributing to pathogenicity are toxins, enzymes and
adhesion. The organism adheres to the epithelial and endothelial cells by
proteinase production. Then the yeast cells of Candida encounter a particular host tissue and colonization takes
place at the local site or they invade deeper into the host tissue and induce
various clinical symptoms.
Clinical Features
The Candida speciesare found as commensal on
mucosal surfaces of the body. They cause disease as and when conditions are
favourable. This yeast like fungi colonizes mucocutaneous surfaces, which can
be portals of entry into deeper tissues when the host defenses are compromised.
They may cause a simple lesion to event the life threatening systemic infection.
The
clinical manifestations of Candidiasis are divided into two broad categories.
They are:
1. Infectious Diseases
a. Mucocutaneous Involvement
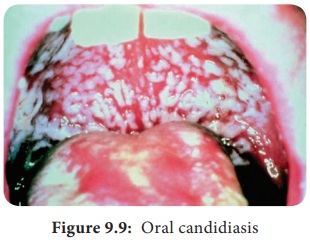
i. Oral Candidiasis – Most common form of Candida
colonizes on the oral cavity. Oral thrush is infection of the buccal mucosa,
gums, tongue. Reddening of the mucous membrane gives dry, smooth metallic taste
and burning at the local site (Figure 9.9).
ii. Alimentary Candidiasis – Candida colonizes
on the oesophagus causing oesophagitis. It is mostly asymptomatic or it may
cause burning pain in the epigastrium or throat.
b. Cutaneous Dermatitis
i. Diaper Dermatitis – Candida that colonize on the cutaneous layer causes
cutaneous Candidiasis, leading to maculopapules vesicles with erythematous
rash. This is common among infants and known as Diaper rash.
ii. Intertrigo
– This is an inflammatory lesion of the skin folds due to
candidal infection.
c. Systemic Involvement
The Candida colonizes in various organs and
causes various manifestations through the blood stream. Clinical features are
found to be Urinary tract Candidiasis,
Candiduria, Endocarditis, Pulmonary
Candidiasis, Arthritis, Osteomyelitis, Meningitis, Candidemia and Septicemia.
2. Allergic Diseases
Allergic
manifestation is caused due to the metabolites of Candida. The cutaneous allergies are urticaria and eczema,
and bronchial asthma.
Laboratory Diagnosis
i. Samples
Specimens collected are mucous membrane
from the mouth, vagina, skin and sputum based on the site of involvement.
a. Direct Examination
Gram
staining LPCB, and KOH wet mount are used to visualize the yeast cells.
Presence
of yeast cells approximately 4.8 µm with budding and pseudo hyphae are
observed. Other stains like periodic acid - Schiff stain and Gomori’s
methylamine silver stain are also used to observe the fungal elements in
tissue.
b. Fungal culture
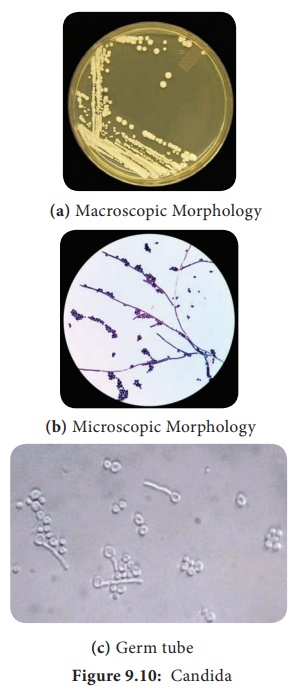
The
clinical specimens can be cultured on Sabouraud dextrose agar (SDA) with
antibiotics and incubated at 25°C and 37°C (Figure 9.10). The colonies appear
in 3–4 days as cream coloured, smooth and pasty.
Some of
the species of Candida are andida albicans, Candida tropicalis, Candida krusei and Candida
glabrata.
ii. Special Test
Germ tube test
The culture of Candida species is treated with sheep or normal human serum and inoculated at 37°C for 2 to 4 hours. A drop of suspension is examined on the slide. The germ tubes are seen as long tube–like projections extending from the yeast cells. The demonstration of the germ tube is known as Reynolds – Braude phenomenon.
Biochemical tests
Sugar
fermentation and assimilation tests are used for the identification of Candidal
species. C.albicans ferments Glucose
and Maltose and assimilates Glucose, Maltose, Sucrose, Lactose and Galactose
Chlamydospores formation
Candida
isolates are grown on corn meal, agar (CHN) or rice starch agar (RSA) and
incubated at 25°C for 2–3 days. The formation of large, thick walled terminal
chlamydospores is demonstrated in C.albicans
and C. dubliniensis.
iii. Treatment
1. 1% gentian violet is locally applied to the
affected areas.
2. The
azole creams like Clotrimazole, Miconazole, Ketoconazole and Econazole are also
used
Cryptococcosis
Cryptococcosis
is an acute, sub acute or chronic fungal disease caused by encapsulated yeast
called Cryptococcus neoformans. It is
pathogenic to man and animals. It
causes opportunistic infection, involving the lungs and disseminates to extra
pulmonary sites through circulation to different body organs particularly to
central nervous system causing Meningoencephalitis.
Infobits.
What does Cryptococcus cause?
Meningitis can be caused by different
germs, including bacteria, fungi,
and viruses. Two types of fungus can cause cryptococcal
meningitis (CM). They are called Cryptococcus neoformans (C. neoformans) and Cryptococcus gattii (C. gattii). This disease is rare in healthy
people.
Pathogenesis and Pathology
Cryptococcal infection occurs through inhalation of small forms or basidiospores. The fungus may remain dormant in the lungs until the immune system weakens and then can disseminate to the central nervous system and other body sites.
Clinical Features
The
clinical features of Cryptococcosis depend upon the anatomical sites.
i. Pulmonary Cryptococcosis
The
respiratory route is usually the portal of entry for propagules in Pulmonary Cryptococcosis
that subsequently disseminate to extra pulmonary sites. The symptoms are dry
cough, dull chest pain and milder or no fever with small gelatinous granules
all over the lungs
ii. CNS Cryptococcosis
This is
an infection of brain and meninges leading to Meningoencephalitis. Nitrogenous
source such as asparagines and creatinine present in cerebrospinal fluid enrich
the yeast. The symptoms are nausea, dizziness, impaired memory, blurred vision
and photophobia. The enlarged granulomatous cerebral lesions are called cryptococcoma.
iii. Visceral Cryptococcosis
This
infection usually spreads from a primary focus to invade the optic nerve and
meninges. Visual loss in patients is due to intra cranial pressure. There are
two distinct patterns of visual loss namely; rapid visual loss (within 12 hrs)
and slow visual loss (within weeks to months).
Laboratory Diagnosis
i. Samples
Specimens
collected are mainly serum, CSF and other body fluids.
a. Direct Examination
10%
Nigrosin or India ink staining, Gram staining and LPCB are used to visualize
the yeast cell.
Biopsy
material is stained with periodic acid - Schiff and Gomoris’s methylamine
silver stain to observe the fungal cells in the tissue. Round budding yeast
cells with a distinct halo gelatinous capsule can be seen (Figure 9.11a). Gram
positive budding yeast cells are demonstrated by Gram staining.
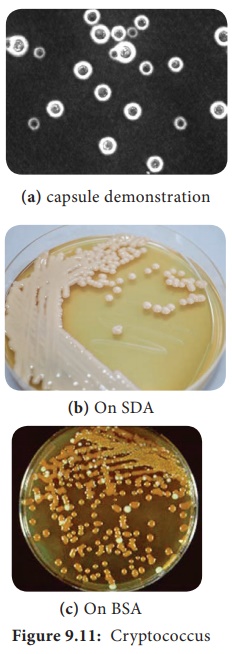
b. Fungal Culture
The
clinical specimens can be cultured on Sabouraud dextrose agar, Bird Seed agar
and incubated at 37°C. The colonies are mucoid, cream to buff - colored in SDA
(Figure 9.11b), whereas brown colored due to conversion of the substrate into
melanin by Phenoloxidase in BSA (Figure 9.11c).
ii. Treatment
1. Amphotericin
B, Flucytosine is given together as induction and maintenance therapy.
2. Fluconazole
is also recommended
Saccharomyces cerevisiae Fungemia: An Emerging Infectious Disease. Saccharomyces S cerevisiae is
well known in the baking and brewing industry andis also used as a probiotic in
humans. However, it is a very uncommon cause of infection in humans.
Related Topics