Chapter: Clinical Dermatology: Physical forms of treatment
Surgery - Physical forms of treatment
Physical forms of treatment
The
skin can be treated in many ways, including surgery, freezing, burning,
ultraviolet radiation and lasers. Some broad principles will be discussed here.
Surgery
As
our population ages, and becomes more concerned about appearances, requests for
skin surgery are becoming more common. The distinction between traditional
dermatological surgery and cosmetic sur-gery is blurring. There are few over
the age of 50 years who do not have a benign tumour that they consider unsightly and wish to have
removed. There are also many who are unhappy with a skin damaged by cumulative
sun exposure, or concerned about medically trivial abnormalities on their face.
To term the treatment of all these as ‘cosmetic’ seems harsh. Health care
systems cannot cover the cost of treating all such problems but family doctors
and dermatologists should be able to discuss with their patients any recent
developments in photo-therapy, laser treatment and specialized surgery that might
help them. For example, doctors should be able to explain that diode lasers can
remove unwanted hair permamently and without visible scarring, and the pros and
cons of such treatment as well as supply-ing the names of specialists expert in
it.
Skin biopsy
The
indications for biopsy, and the techniques employed, are described in Earily.
Excision
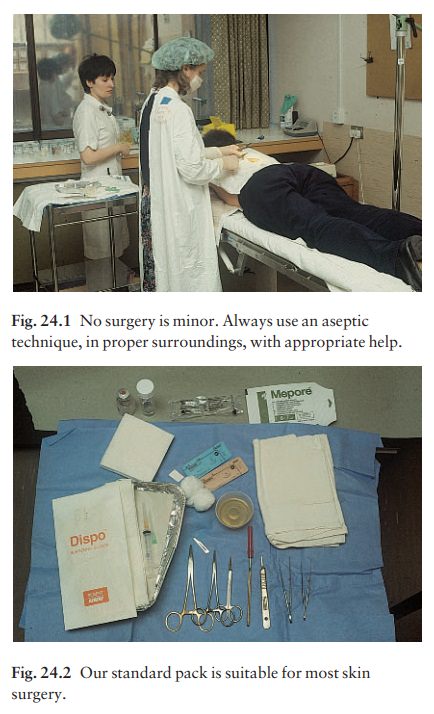
Excision
under local anaesthetic, using an aseptic technique, is a common way of
removing small
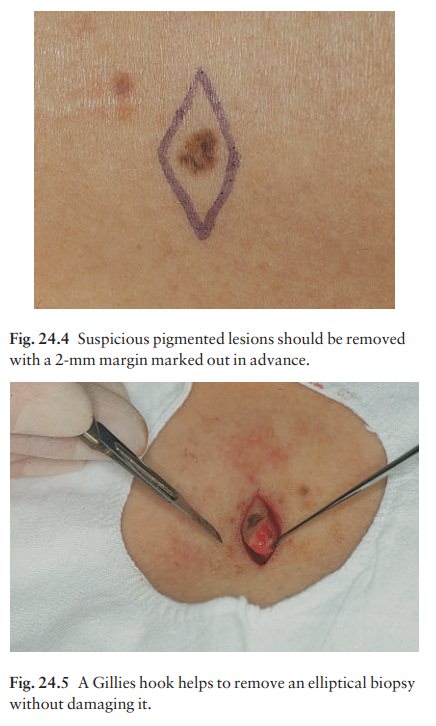
After injection of the local anaesthetic [usually 1 or 2% lignocaine
(lidocaine) with or without 1 in 200 000 adrenaline (epinephrine);], the lesion
is excised as an ellipse with a margin of normal skin, the width of which
varies with the nature of the lesion and the site (Fig. 24.4). The scalpel
should be held perpendicular to the skin surface and the incision should reach
the subcutaneous fat. The ellipse of skin is carefully removed with the help of
a skin hook (Fig. 24.5) or fine-toothed forceps. Larger wounds, and those where
the scar is likely to stretch (e.g. on the back), are closed in layers with
absorbable sutures (e.g. Dexon) before apposing the skin edges without tension
using non-absorbable interrupted or continu-ous subcuticular sutures such as nylon
or Prolene. Stitches are removed from the face in 4–5 days and from the trunk
and limbs in 7–14 days. Artificial sutures (e.g. Steri-Strip) may be used to
take the tension off the wound edges after the stitches have been taken out.
Shave excision
Many
small lesions are removed by shaving them off at their bases with a scalpel
under local anaesthesia. This procedure is suitable only for exophytic tumours
that are believed to be benign. Some cells at the base may be left and these,
in the case of malignant tumours, would lead to recurrence.
Saucerization excision
This modified shave excision extends into the sub-cutaneous fat. It is used to remove certain small skin cancers and worrying melanocytic naevi. It leaves more scarring than a shave excision but the technique provides tissue that allows the dermatopathologist to determine if a tumour is invading and to measure tumour thickness if the lesion is a melanoma. Further-more, the technique may ensure complete removal more adequately than shave excision.
Curettage
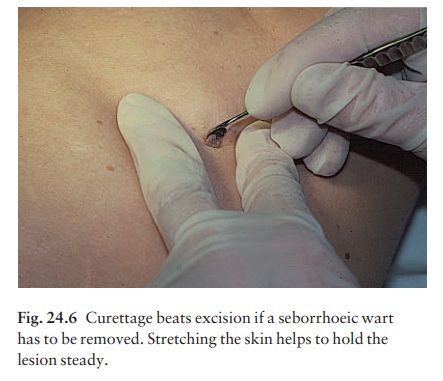
Curettage
under local anaesthetic is also used to treat benign exophytic lesions (e.g.
seborrhoeic keratoses; Fig. 24.6) and, combined with electrodesiccation , to
treat some basal cell carcinomas. Its main advantage over purely destructive
treatment is that histological examination can be carried out on the curettings.
A sharp curette is used to scrape off the lesion and haemostasis is achieved by
local haema-tinics, by electrocautery or electrodesiccation. The wound heals by
secondary intention over 2–3 weeks, with good cosmetic results in most cases.
When
a basal cell carcinoma is treated, the curette is scraped firmly and thoroughly
along the sides and bottom of the tumour (the surrounding dermis is tougher and
more resistant to curettage than the carcinoma) and the bleeding wound bed is
then elec-trodesiccated aggressively. This stops bleeding and destroys a zone
of tissue under and around the excised tumour to provide a tumour-free margin.
The process is repeated once or twice at the same session to ensure that all of
the tumour has been removed or destroyed. Only small basal cell carcinomas
outside the skin folds should be treated in this way. The recurrence rates are
relatively high for tumours in the nasolabial folds, over the inner canthi and
on the nose, glabella and lips. The technique should not ordinarily be usedfor
sclerosing basal cell carcinomas, invasive lesions larger than 1–2 cm, rapidly
growing tumours or for those with micronodular features on histology.
Microscopically controlled excision (Mohs’ surgery)
This
form of surgery for malignant skin tumours is time-consuming and expensive, but
the probability of cure is greater than with excision or curettage. First, the
tumour is removed with a narrow margin. The excised specimen is then marked at
the edges, mapped and, after rapid histological processing, is immediately
examined in horizontal and vertical section. If the tumour extends to any
margin, further tissue is removed from the appropriate place, based on the
markings and mappings, and again checked histologically. This process is
repeated until clearance has been proved histologically at all margins. The
resulting wound can then be closed directly, covered with a split skin graft or
allowed to heal by secondary intention.
Mohs’
surgery is useful to treat:
•
a basal cell carcinoma with a poorly
defined edge;
•
a sclerosing basal cell carcinoma
(can suggest an enlarging scar clinically);
•
a recurrent basal cell carcinoma;
•
a basal cell carcinoma lying where
excessive mar-gins of skin cannot be sacrificed to achieve complete removal of
the tumour (e.g. one near the eye);
•
basal cell carcinomas in areas with
a high incidence of recurrence such as the nose, glabella or nasolabial folds;
•
some squamous cell carcinomas; and
•
occasional malignant tumours other
than basal and squamous cell carcinomas.
Flaps and grafts
These
can be used to reconstruct a defect left by the wide excision of a tumour, or
when a tumour is removed at a difficult site, e.g. the eyelid or tip of the
nose.
Electrosurgery
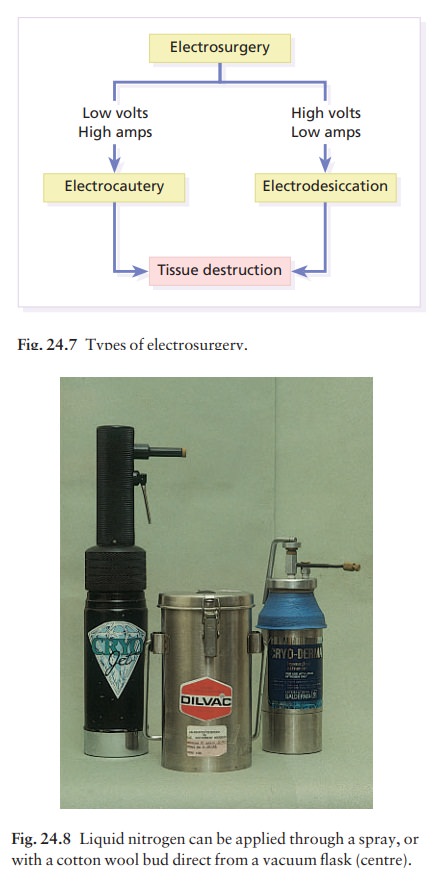
This
is often combined with curettage, under local anaesthesia, to treat skin tumours.
The main types are shown in Fig. 24.7.
Related Topics