Chapter: Pathology: Gastrointestinal Tract Pathology
Small and Large Intestines
SMALL AND LARGE INTESTINES
Mechanical Obstruction
Volvulus is a twisting of a segment of bowel on its
vascular mesentery, causing intestinal obstruction and infarction. It is often
associated with congenital abnormalities such as intestinal malrotation. Common
locations include the sigmoid colon and small bowel; complications include
infarction and peritonitis.
Intussusception is the telescoping of a proximal
segment of the bowel into the distal segment. It is most common in infants and
children. Children present with vomiting, abdominal pain, passage of blood per
rectum, and lethargy; a sausage-shapedmass is often palpable in the right
hypochondrium.
In adults, intussusception may be caused by a mass
or tumor. The intussusceptedsegment can become infarcted.
Incarcerated hernia is a segment of bowel that is
imprisoned within a hernia; the condition can become complicated by intestinal
obstruction and infarction.
Hirschsprung disease (or
congenital aganglionic megacolon) is caused by congenital absence of ganglion cells in the rectum
and sigmoid colon, resulting in intestinal obstruction. The condition affects
males more than females, and can be associated with Down syndrome. Hirschsprung
may present with delayed passage of meco-nium, or with constipation, abdominal
distention, and vomiting.
Grossly, the affected segment
is narrowed, and there is dilation proximal to the narrow segment (megacolon).
Microscopically, there is an absence of ganglion cells in Auerbach and Meissner
plexuses, and the diagnosis is established when rectal biopsy demonstrates the
absence of ganglion cells. Treatment is resection of the affected segment.
Malabsorption Syndromes
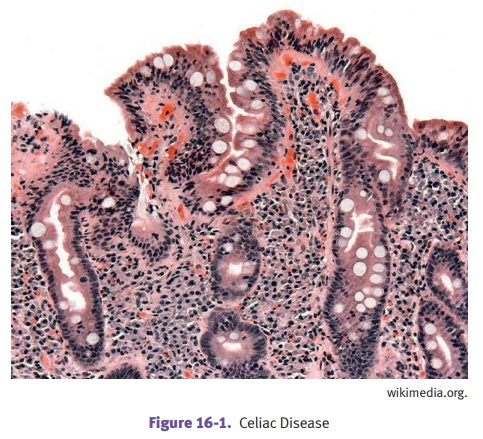
Celiac sprue (or gluten-sensitive enteropathy and
nontropical sprue) is caused by hypersensitivity to gluten
(and gliadin), resulting in loss of small bowel villi and malabsorption.
HLA-DQ2 and/or -DQ8 are carried by most patients. Microscopic exam demonstrates
a loss of villi, with increased intraepithelial lymphocytes and increased
plasma cells in the lamina propria.
Clinically, it often presents
in childhood with malabsorption. Symptoms include abdominal distention,
bloating, and flatulence, along with diarrhea, steatorrhea, and weight loss.
Dermatitis herpetiformis may occur age >20. In adults, celiac presents
between decades 4-7. Treatment is dietary restriction of gluten. There is an
increased risk of gastrointestinal cancer.
Environmental enteropathy (previously known as tropical sprue) is a maladaptive disease of unknown etiology (infection and/or
nutritional deficiency). If affects resi-dents of low-income countries. Biopsy
shows blunting of villi and a lymphocytic infiltrate.
Whipple disease is a rare infectious disease
involving many organs, including small intestines, joints, lung,
heart, liver, spleen, and central nervous system. It typically affects
Caucasian males age 30-50.
The infecting organism is Tropheryma whipplei. Microscopically,
the small bowel lamina propria is filled with macrophages stuffed with the PAS
-positive, gram-positive, rod-shaped bacilli. Patients present with
malabsorption, weight loss, and diarrhea. Treatment is antibiotics.
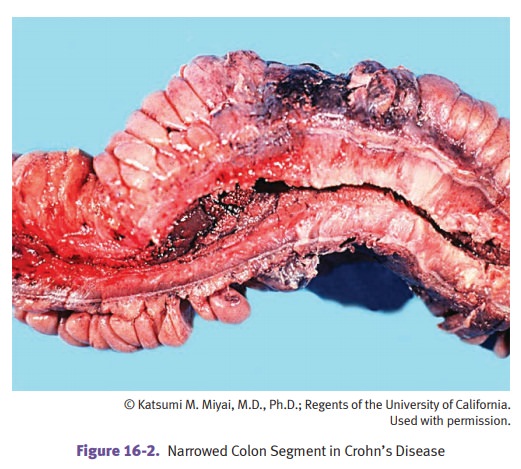
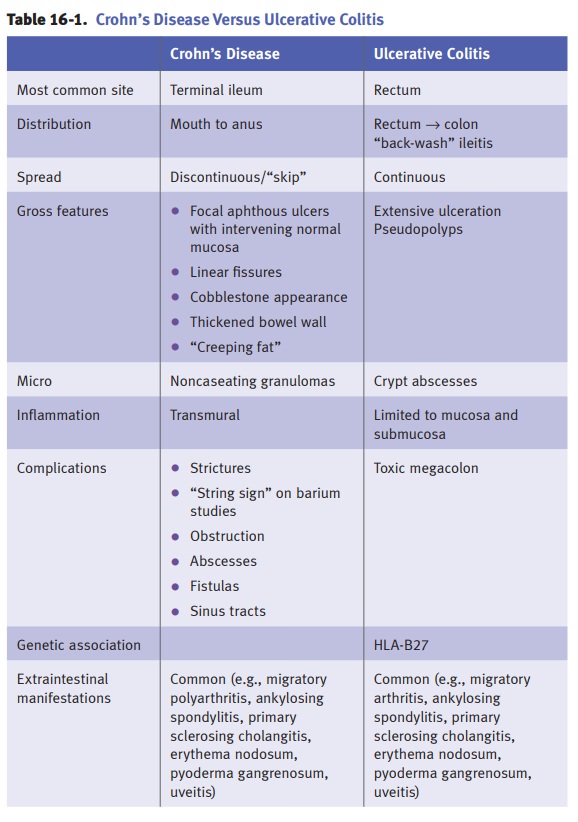
Inflammatory bowel disease (IBD). There are 2 categories of
IBD:
•
Crohn’s
disease (CD) (or regional enteritis)
•
Ulcerative
colitis (UC)
Colitis of indeterminate type
describes cases that cannot be clearly classified.
Caucasians develop IBD more
frequently than non-Caucasians. The incidence of IBD is increasing.
Age distribution varies with
the disease:
•
CD has a bimodal distribution with peaks at age 10–30 and 50–70
•
UC peaks at age 20–30
IBD can present with episodes
of bloody diarrhea or stools with mucus, crampy lower abdominal pain, or fever.
CD may present with malabsorption or extraint-estinal manifestations. It may
mimic appendicitis. CD may cause perianal fistulas.
Diagnosis of IBD requires
endoscopic biopsy and clinicopathologic correlation.
New studies indicate that
risk of colorectal carcinoma (CRC) in CD and UC are equivalent for similar
extent and duration of disease; the risk of CRC is not as high as previous
studies suggested.
Miscellaneous Conditions
Ischemic bowel disease is caused by decreased blood
flow and ischemia of the bowel, secondary to atherosclerosis
with thrombosis, thromboembolism, or reduced car-diac output from shock. It is
most common in older individuals. Typical presenta-tion is with abdominal pain
and bloody diarrhea. The disease distribution tends to involve watershed areas
(e.g., splenic flexure), and affected areas typically show hemorrhagic
infarction.
Treatment is surgical
resection, but the prognosis is poor, with >50% mortality.
Hemorrhoids
are
tortuous, dilated anal submucosal veins caused by increased venous pressure. Risk factors
include constipation and prolonged straining during bowel movements, pregnancy, and cirrhosis.
Complications include painful thrombosis and streaks of bright red blood on
hard stool.
Angiodysplasia is arteriovenous
malformations of the intestines. It occurs in the cecum and right colon.
Individuals age >55 are most commonly affected, presenting with multiple
episodes of rectal bleeding. It is associated with Osler-Weber-Rendu and CREST
syndromes. Treatment is surgical resection.
Melanosis coli is common with laxative
abuse; it causes black pigmentation of the colon due to the ingestion of
the laxative pigment by macrophages in the mucosal and submucosa. It can mimic
colitis or malignancy.
Pseudomembranous colitis (antibiotic-associated
colitis) is an acute colitis charac-terized by the formation of inflammatory
pseudomembranes in the intestines. It is usually caused by Clostridium difficile infection (often brought on by a course of
broad-spectrum antibiotics, especially clindamycin and ampicillin), but it can
be caused by ischemic bowel disease.
Gross examination shows
yellow-tan mucosal membranes. Microscopic exam shows the pseudomembranes are
composed of an adherent layer of acute inflammatory cells, mucus and necrotic
debris overlying sites of colonic mucosal injury. Presenta-tion is with
diarrhea, fever, and abdominal cramps. Diagnosis is established with detection
of C. difficile toxin in the stool.
Treatment of clostrial pseudomembranous colitis is vancomycin or metronidazole.
Appendicitis is most commonly caused by obstruction of the
appendix by a feca-lith. It often starts with periumbilical pain that
subsequently localizes to the right lower quadrant. Nausea, vomiting, and fever
may also be present. Lab studies show an elevated white blood cell count. A
complication is appendiceal rupture leading to peritonitis. Grossly, a
fibrinopurulent exudate may be seen on the appendiceal serosa; microscopically,
neutrophils are present within the mucosa and muscular wall (muscularis
propria) of the appendix.
Diverticula
Meckel diverticulum is a congenital small bowel
diverticulum caused by persistance of a remnant of the vitelline
(omphalomesenteric) duct. With Meckel, the “rule of 2s” applies:
•
2% of the normal population
•
2 feet from the ileocecal valve
•
Length 2 cm
•
Age ≤2 years at time of diagnosis
Most Meckel diverticula are
asymptomatic but they may contain rests of ectopic gastric mucosa and present
with intestinal bleeding.
Colonic diverticulosis is an acquired outpouching of
the bowel wall, characterized by herniation of the mucosa
and submucosa through the muscularis propria (pseu-dodiverticulum). It is
extremely common in the United States.
•
Incidence increases with age
•
Major risk factor is a low-fiber diet, which leads to increased
intraluminal pressure
•
Most common location is sigmoid colon
Many cases are asymptomatic
and picked up on screening colonoscopy. When symptomatic, it can cause
constipation alternating with diarrhea, left lower quad-rant abdominal cramping
and discomfort, occult bleeding and an iron deficiency anemia, or lower
gastrointestinal tract hemorrhage. Complications include diver-ticulitis,
fistulas, and perforation with accompanying peritonitis.
Polyps
Hamartomatous polyps include nonfamilial juvenile
polyps and polyps associated with a familial
(Peutz-Jeghers) syndrome. Nonsyndromic polyps do not have malig-nant potential.
Hyperplastic polyps are the most common
histologic type; they occur most often in the left colon and are
usually <5 mm. Although previously considered not to have malignant
potential, newer studies suggest they are part of a group of polyps with
serrated histology and risk of progression to cancer. Serrated polyps occur more often in the
right colon.
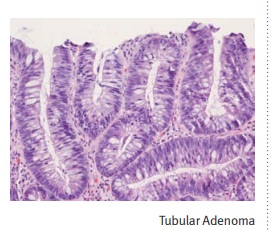
Tubular and villous adenomas have long been known to have
malignant potential. Microscopically, they show
cellular dysplasia and either pure tubular, pure villous or tubulovillous
histology.
Familial Syndromes
Familial adenomatous polyposis (FAP), also called
adenomatous polyposis coli (APC), is due to an autosomal
dominant mutation of the APC gene on
chromo-some 5q21.
Affected individuals may
develop thousands of colonic adenomatous
polyps; the diagnosis is made with discovery of >100 adenomatous polyps
on endoscopy. Com-plications: by age
40, virtually 100% will develop an invasive adenocarcinoma and increased risks for developing
duodenal adenocarcinoma and adenocarcinoma of the papilla of Vater.
Gardner syndrome is an autosomal dominant
variant of familial adenomatous pol-yposis characterized by numerous colonic
adenomatous polyps, multiple osteomas, fibromatosis, and epidermal inclusion
cysts.
Turcot syndrome is a rare variant of familial
adenomatous polyposis character-ized by numerous colonic adenomatous polyps and
central nervous system tumors (gliomas).
Hereditary nonpolyposis colorectal cancer (HNPCC), or Lynch syndrome,
is due to an autosomal dominant mutation of a DNA
nucleotide mismatch repair gene that predisposes for colon cancer. It is
associated with an increased risk of cancer at other sites, including the
endometrium and the ovary.
Peutz-Jeghers syndrome is an autosomal dominant
condition characterized by mul-tiple hamartomatous polyps (primarily in the
small intestine); melanin pigmenta-tion of the oral mucosa; and increased risk
of cancer at numerous sites including the lung, pancreas, breast, and uterus.
Neoplasia
Colonic adenocarcinoma is the third most common
tumor in the United States, in terms of incidence and
mortality. Risk factors include:
•
Dietary factors (low fiber, low fruits/vegetables and high in red
meat and animal fat)
•
Colon polyps (isolated adenomatous polyps, hereditary polyposis
syndromes)
•
Other colon disease (Lynch syndrome, ulcerative colitis)
Diagnosis is established via
endoscopy with biopsy.
Cancer genetics: Mutations of the APC gene cause activation of the Wnt pathway, leading β-catenin to translocate to the nucleus where it causes
the overexpression of growth-promoting genes. DNA mismatch repair causes
microsatellite instability, which is another genetic carcinogenesis pathway.
The pattern of spread in
colonic adenocarcinoma includes lymphatic spread to mes-enteric lymph nodes,
with distant spread to liver, lungs, and bone. Staging is with the TNM system.
Treatment can include surgical resection and chemotherapy (for metastatic
disease); CEA levels can be used to monitor for disease recurrence.
Screening is recommended for
the general population beginning age 50. Current guidelines suggest:
•
Colonoscopy every 10 years or annual fecal occult blood test
(FOBT), or
•
Combination of FOBT (every 3 years) and sigmoidoscopy (every 5
years)
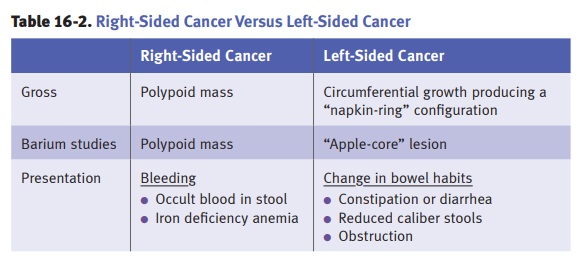
Table
16-2.
Carcinoid tumors are neuroendocrine tumors
that often produce serotonin. Loca-tions include the appendix (most common) and
the terminal ileum. Metastasis to the liver may result in carcinoid heart
disease.
Carcinoid syndrome is characterized by diarrhea,
cutaneous flushing, bronchospasm and wheezing, and fibrosis.
The diagnosis is substantiated by demonstrating elevated urinary 5-HIAA
(5-hydroxyindoleacetic acid).
Gastrointestinal stromal tumor (GIST) is the most common sarcoma of
the GI tract. Most cases have a KIT mutation. The peak incidence is in
decade 7. Treatment is resection and a tyrosine-kinase inhibitor.
Related Topics