Chapter: Pathology: Gastrointestinal Tract Pathology
Esophagus
ESOPHAGUS
Congenital and Mechanical Disorders
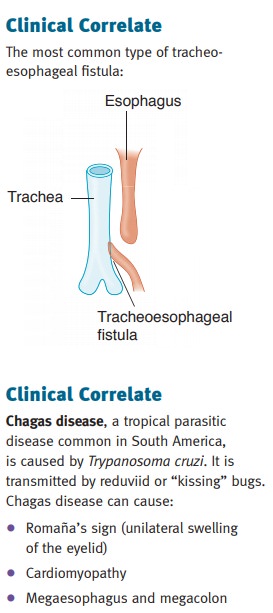
Tracheoesophageal fistula may arise as a congenital
connection between the esopha-gus and trachea that is often associated with
esophageal atresia. It is often discovered soon after birth because of
aspiration. In adults the condition can occur secondary to malignancy, trauma,
or iatrogenic causes.
Esophageal webs are web-like protrusions of
the esophageal mucosa into the lumen which typically present with
dysphagia. Plummer-Vinson syndrome is a disease of middle-aged women
characterized by esophageal webs, iron deficiency anemia, and increased risk of
carcinoma. Schatzki rings are web-like narrowings at the gastro-esophageal
junction.
Achalasia is a failure of the lower esophageal sphincter
(LES) to relax with swallow-ing. The etiology is unknown in most cases; in
South America, achalasia may be caused by Chagas disease. Presentation is with
progressive dysphagia. The esopha-gus is characteristically dilated proximal to
the lower esophageal sphincter; barium swallow shows a “bird-beak” sign.
Microscopically, there is a loss of ganglion cells in the myenteric plexus.
Treatment is LES balloon dilation or myotomy. Achalasia carries an increased
risk for esophageal carcinoma.
Hematemesis and Esophageal Bleeding
Mallory-Weiss syndrome is esophageal bleeding due to
linear lacerations at the gas-troesophageal junction from severe prolonged
vomiting; the most common cause is acute alcohol ingestion and/or chronic
alcoholism. Esophageal rupture (Boerhaave syndrome) may result.
Esophageal
varices are dilated submucosal veins in the lower third of the esophagus, usually secondary to portal
hypertension. The most common cause is cirrhosis. Clinically, the presentation
is asymptomatic, though there is massive hematemesis when the varices are
ruptured. Complications include potentially fatal hemorrhage. Treatment is
generally band ligation, sclerotherapy, or balloon tamponade.
Esophagitis
Gastroesophageal reflux disease (reflux
esophagitis) (GERD) is esophageal irritation and inflammation due to
reflux of gastric secretions into the esophagus. Reflux typi-cally presents
with heartburn and regurgitation. Complications include bleeding, stricture,
bronchospasm and asthma, and Barrett esophagus.
Barrett esophagus is a metaplasia of the
squamous esophageal mucosa to a more protective columnar type
(intestinal metaplasia). It occurs because of chronic expo-sure to gastric
secretions, usually in the setting of GERD. The endoscopic appearance is of an
irregular gastroesophageal junction with tongues of red granular mucosa
extending up into the esophagus. Barrett has an increased risk for dysplasia
and esophageal adenocarcinoma. The incidence of Barrett esophagus is increasing
in the United States.
Esophageal Carcinoma
Squamous
cell carcinoma (SCC) of the esophagus is the most common type of esophageal cancer in the
world. It affects males more than females, and African Americans more than
Caucasians; typical age is usually age >50. Risk factors include:
•
Heavy smoking and alcohol use
•
Achalasia
•
Plummer-Vinson syndrome
•
Tylosis
•
Lye ingestion
The presentation of squamous
cell carcinoma of the esophagus varies; it is often asymp-tomatic until late in
the course. When symptoms do develop they may include progres-sive dysphagia,
weight loss and anorexia, bleeding, hoarseness, and cough. Diagnosis is by
endoscopy with biopsy. Treatment is surgery though the prognosis is poor.
Adenocarcinoma of the esophagus affects Caucasians more than
African Ameri-cans. It arises in the distal esophagus. The progression from
Barrett metaplasia to dysplasia and eventually to invasive carcinoma occurs due
to the stepwise accumula-tion of genetic and epigenetic changes. The prognosis
is poor.
In the United States, adenocarcinoma
and squamous cell carcinoma of the esophagus occur with equal frequency.
Related Topics