Chapter: Medicine Study Notes : Public Health
Screening
Screening
Definitions
· Screening:
o The presumptive identification of unrecognised/preclinical disease or
defects by the application of tests, examinations or other processes that can
be applied rapidly (and cheaply)
o Sorts people into high and low risk groups for further diagnosis of high
risk.
o Is NOT diagnostic on its own
·
Mass/population Screening:
systematic screening of populations
·
Opportunistic screening:
Non-systematic, when the opportunity arises
·
Selective Screening: systematic
screening of high risk groups
·
Screening test: a test performed
without a clinical indication
·
Objectives of screening:
o ¯Mortality/morbidity
from disease on the individual
o Limit the impact of disease on a community
o Identify compensatable disability (eg poor eyesight in kids)
Criteria for Screening Programmes
·
Is the disease an important
health problem (incidence, impact, preventability)
·
Is a suitable screening test available:
o Acceptable, simple,
o High sensitivity, as specific as possible
o PPV: probability that a person with a positive test does have the
disease, depends on sensitivity, specificity AND prevalence
o NPV: probability that a person with a negative test does not have the
disease
o Yield (proportion of cases of the disease accurately identified by a
screening test),
o Repeatability (depends on variation in method, subject variation,
observer variation)
·
Is the natural history of the
disease well understood:
o A recognisable latent or early symptomatic stage
o The length of the asymptomatic stage determines screening frequency. Is
this long enough to make the screening interval reasonable?
·
Does screening lead to
interventions that improve quality of life:
o Does early intervention offer benefits over later intervention
o Accepted treatment, proven effectiveness. Ideally want an RCT that demonstrate screening verses no screening improves mortality/morbidity
·
Is there an appropriate
infrastructure available to provide screening and follow-up services:
o Are there pilot studies demonstrating how it should work?
o Is there local and national support?
o Are the services accessible (in terms of geographic, cultural barriers, cost), does the system have sufficient capacity, and is there appropriate quality control processes in place
·
Is the screening programme cost
effective?
Screening Test
· Eg PSA for prostate cancer, intra-ocular pressure for glaucoma, etc
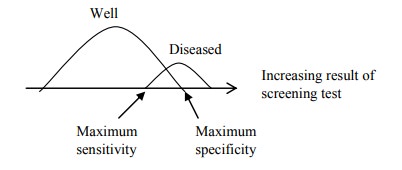
· For a screening test, you want a test that maximises sensitivity: maximise true positives (minimises false negatives), so that you identify all diseased cases. The downside is an increasing rate of false positives who have unnecessary further investigation
· A highly specific test would maximise true negatives (ie minimise positives, so would not further test anyone unnecessarily), but at the cost of increasing false negatives – who are the people you actually want to detect
· See also Topic: Evaluation of Diagnostic Tests
Biases
· Lead-time bias: interval from detection to point where diagnosis would have been made without screening. Depends on length of pre-clinical phase, frequency of testing, and the test sensitivity
·
Length bias: Cases with a disease
with a longer natural history are more likely to be detected by a screening
programme. But these cases also have a better prognosis. Thus screening leads
to a better prognosis, regardless of whether screening itself confers any
benefits
·
Selection bias: selection,
referral or volunteer bias results in a selected subset of the population being
screened
Screening Programmes in NZ
·
National screening programmes:
o Neonates: inborn errors of metabolism – Guthrie Card
o Cervical Cancer
o Vision/hearing testing at school entry (erratic)
o Mammography
·
Controversial and not currently
recommended population screening programmes:
o Prostate (PSA)
o Colorectal cancer
o Otitis media with effusion
·
Current screening pilots:
Hepatitis B
·
Opportunistic screening
o Antenatal screening
o Blood pressure
o Cholesterol
o Blood glucose
o HIV
o Osteoporosis
o Glaucoma, etc
· Deciding to implement a screening programme:
o The decision to implement a population based screening programme is complex, must be justified on the basis of standard WHO criteria and supported by research evidence
o The rules to do with population health are NOT those of an individual clinician (ie just because you would screen an asymptomatic man for prostrate cancer is not a reason to implement a national programme)
o Potential to do harm at a population level is considerable („first do no
harm‟)
o We are „imposing‟ something – need sound evidence
Ethical Considerations
· Costs and benefits:
o Costs should include adequate support, counselling, etc. Benefits should include quality of life (but subjective)
o Many harms are personal – false alarm, false reassurance. Difficult to account for
·
Justice:
o Distribution: benefits accrue to a few and are large; harms fall on many and are minor. Is this fair?
o Inconvenience borne by many to benefit the few – but this also benefits the group (social welfare function)
o Collective gains depend on high levels of individual participation
·
Autonomy:
o Motivation: altruism only effective if participants well
informed/educated
o Imposition: Opt-out strategies – trade-off between recruitment level and
maximal choice
o Results: safeguards on third party disclosure
·
Opportunistic screening:
o Cost and benefit usually borne by the same individual
o Offered responsively rather than proactively
o Appropriate treatment or other follow-up available
· For Prostate Screening, see Prostate Cancer Screening. Prepared for Public Health test.
Related Topics