Chapter: Medicine Study Notes : Public Health
Health Economics
Health Economics
·
= The study of how individuals
and societies, experiencing virtually limitless wants, choose to allocate scare
resources to best satisfy their wants
·
Scarcity:
o Resources (main factors of production – natural resources, capital, labour) are scare
o ® Goods
and services produced from them are scarce
o Can‟t have as much as we would want if they are free
o Will always be medical interventions that cannot be funded
·
Choice: Because of scarcity, we
must make choices
· Opportunity cost:
o The loss of the next best opportunity we could have chosen (ie if we use time/money on one thing, it‟s not available for something else)
o When doing an evaluation: deduct GST (it‟s a transfer), use real price (eg not subsidised cost of a drug), include indirect costs (eg patient travel)
o Can be calculated from different perspectives: eg provider, funder,
society
·
Marginal analysis:
o = Incremental benefit (ie marginal benefit) from incremental cost (ie
marginal cost)
o Decisions are usually about whether to expand or contract – not stop or
start
o Marginal cost is NOT the same as average cost
·
Efficiency:
o = Maximising benefits from certain cost of inputs
o Not the same as cost-cutting: if you cut costs and output falls then
haven‟t improved efficiency
o Effectiveness: are patients better off (eg have better health) with
intervention than without
o Technical efficiency: providing effective services at least cost – doing things right
o Allocative efficiency: concentrating resources on effective services
that offer the biggest payoff in terms of health – doing the right things
o Inefficiency is unethical (if budget is constrained)
·
Equity:
o = Fairness: usually of distribution or payment
o Equal access for equal need (what is need – ill health or capacity to benefit)
o Equal resources for equal need (same amount of money for equal needs –
basis of the DHB funding formula)
o Equal outcomes: allocate resources to achieve same health status of
different populations
·
Markets:
o Means of allocating scarce resources
o Result from the interaction of demand and supply, mediated by price
o Consumers can signal demands, maximise their „well-being‟ or utility,
producers can shift resources accordingly
o If there is perfect competition, theoretically you get allocative
efficiency
o For this to work, requires:
§ Perfect information (eg about quality, costs, etc)
§ No externalities (someone else bears a cost or benefit)
§ Goods and services must be rival in consumption (ie if I buy it no one
else can have it) and excludable (you can‟t have it if you can‟t pay)
§ Freedom of entry and exit
§ Perfect competition – no monopolies
§ No supplier-induced demand
§ Equity is not an issue (ie no merit goods – goods that society believes
should be more widely available than would occur through markets alone)
o Market failure in health care:
§ Externalities eg immunisation
§ Monopolies eg secondary services, labour markets
§ Asymmetric information eg health professionals
§ Supplier induced demand (especially if fee-for-service)
§ Highly inelastic demand
o Health Insurance Markets
§ Uncertainty about future health needs + high costs ® demand for insurance
§ Moral Hazard: will now consume more health care than they otherwise would as someone else is paying (can control with co-payments)
§ Adverse selection: patients who know they will need it are more likely to purchase it. Insurers won‟t know so premiums won‟t reflect risk
o Want to getting advantages of market efficiency and overcoming market
failure ® ?government failure, purchaser provider splits, quasi markets (health
care plans)
·
International Comparisons: Health Expenditure per capita and GDP. NZ is on the line
·
Economic Evaluations :
o = Comparative analysis of alternative courses of action in terms of
their costs and consequences
o Informs choices about the allocation of scarce resources
o Needed to determine efficacy (in lab conditions), effectiveness (more
good than harm in practice)
o Can be prospective or retrospective
o Types of evaluation:
§ Cost minimisation: compare inputs, assume outputs are equal
§ Cost benefit: compares different outcomes (eg flu jabs and hypertension screening). Convert to common unit ($) to compare – but can human life be valued?
§ Cost effectiveness: relates cost to a clinical measure (eg ¯blood pressure, morbidity, life years gained). Has superseded cost-benefit analysis due to problems allocating monetary values to all outputs
§ Cost utility: cost per QALY gained. Can compared across a whole range of interventions ut methodological problems. Example: Impact on QALYs of dialysis verses kidney transplant.
·
Common approaches to valuing
human life:
o Human capital: future earnings (but elderly have none)
o Implied valuations: value implicit in past policies
o Insurance values: but this is paid to survivors
o Willingness to pay to reduce low probability of death: survey or observe
(eg how much do people spend on safety)
·
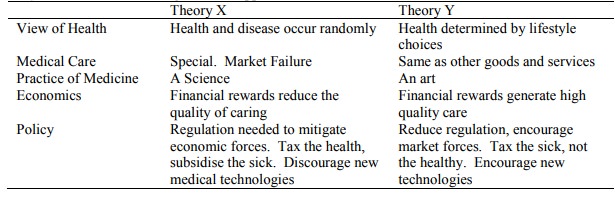
Theory X and Y: Summarising different approaches to health
care in health economics
Related Topics