Chapter: Ophthalmology: Sclera
Sclera : Inflammations
Inflammations
Inflammations are the most clinically
significant scleral changes encountered in ophthalmologic practice. They more
often involve the anterior sclera (epis-cleritis and anterior scleritis) than
the posterior sclera (posterior scleritis).
Classification:
Forms of scleral inflammation are differentiated as follows:
❖ Location: anterior or posterior, i.e., anterior or posterior to the
equator ofthe globe.
❖ Depth:
–
Superficial (episcleritis).
– Deep
(scleritis).
❖ Nature:
–
Diffuse (usually scleritis).
–
Circumscribed or segmental (episcleritis).
– Nodular, with formation of small mobile nodules (scleritis and epis-cleritis).
–
Necrotizing (scleritis only).
–
Non-necrotizing (scleritis only).
Episcleritis
Definition
Circumscribed, usually segmental, and
generally nodular inflammation of the
episclera (connective tissue between sclera and conjunctiva).
Epidemiology:
Episcleritis is the most common form of scleral inflammation.
Etiology:
Episcleritis is rarely attributable to one of
the systemic underlyingdisorders listed in Table 6.1, and is only occasionally due to bacterial or viral inflammation.
Often episcleritis will have no readily discernible cause.
Symptoms:
Episcleritis can be unilateral or bilateral.
It is usually associatedwith segmental reddening and slight tenderness to
palpation.
Findings:
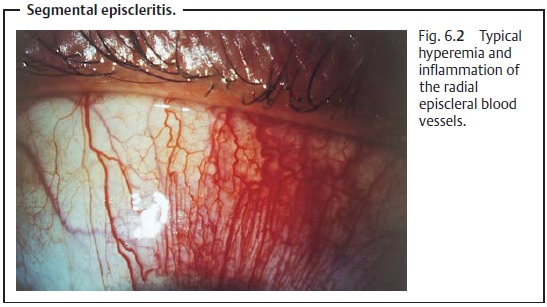
The episcleral vessels lie within the fascial
sheath of the eyeball(Tenon’s capsule) and are arranged radially. In
episcleritis, these vessels and the conjunctival vessels above them become
hyperemic (Fig. 6.2). Tenon’s
capsule and the episclera are infiltrated with inflammatory cells, but the
sclera itself is not swollen. The presence of small mobile nodules is typical of nodular episcleritis.
Differential diagnosis:
The disorder should be distinguished from
con-junctivitis (see next paragraph) and scleritis (6.6.2).
The conjunctival blood vessels are the most
superficial; the episcleral vessels lie within Tenon’s capsule and are arranged
radially. When vaso-constrictive eyedrops are applied, the conjunctival
injection will disap-pear but not the episcleral injection. This makes it
possible to distin-guish conjunctivitis from episcleritis.
Treatment and prognosis:
Episcleritis usually resolves
spontaneouslywithin one to two weeks, although the nodular form can persist for
extended periods of time. Severe symptoms are treated with topical steroids
(eyedrops) or with a nonsteroidal anti-inflammatory agent.
Scleritis
Definition
Diffuse or localized inflammation of the
sclera. Scleritis is classified according to location:
❖ Anterior (inflammation anterior to the equator of the globe).❖ Posterior (inflammation posterior to the equator of the globe).Anterior
scleritis is further classified according to its nature:
❖ Non-necrotizing anterior scleritis (nodular or diffuse).
❖Necrotizing anterior scleritis (with or without inflammation).
Epidemiology:
Scleritis is far less frequent than
episcleritis. Patients are gen-erally older, and women are affected more often
than men.
Etiology:
Approximately 50% of scleritis cases (which
tend to have severeclinical courses) are attributable to systemic autoimmune or
rheumatic dis-ease (Table 6.1), or
are the result of immunologic processes associated with infection. This applies
especially to anterior scleritis. Posterior scleritis is not usually associated
with any specific disorder. As with episcleritis, scleritis is only
occasionally due to bacterial or viral inflammation.
Symptoms and findings:
All forms except for scleromalacia perforans
areassociated with severe pain and
general reddening of the eye.
Anterior non-necrotizing scleritis (nodular form).The nodules consist ofedematous swollen sclera and are not mobile (in contrast to episcleritis).
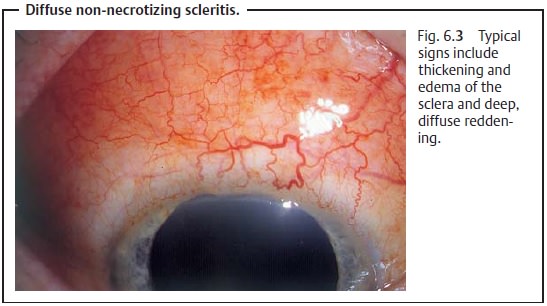
Anterior necrotizing scleritis (diffuse form).The inflammation is moresevere than in the
nodular form. It can be limited to a certain segment or may include the entire
anterior sclera (Fig. 6.3).
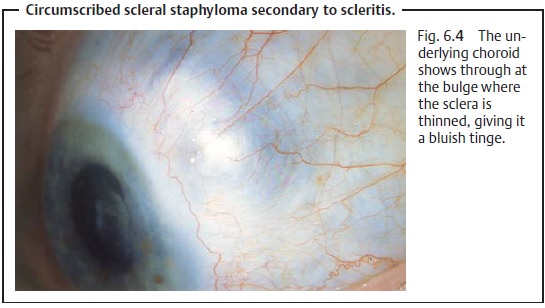
Anterior necrotizing scleritis with inflammation.Circumscribed reddeningof the eyes is a
typical sign. There may be deviation or injection of the blood vessels of the
affected region, accompanied by avascular patches in the episcleral tissue. As
the disorder progresses, the sclera thins as the scleral lamellae of collagen
fibrils melt, so that the underlying choroid shows through (Fig. 6.4). The inflammation gradually spreads
from its primary focus. Usually it is associated with uveitis.
Anterior necrotizing scleritis without inflammation (scleromalacia per-forans).This form of scleritis typically occurs infemale patientswith a longhistory of seropositive rheumatoid arthritis. The clinical course of the dis-order is usually asymptomatic and begins with a yellow necrotic patch on the sclera. As the disorder progresses, the sclera also thins so that the underlying choroid shows through. This is the only form of scleritis that may be painless.
Posterior scleritis.Sometimes there will be no abnormal findings in the ante-rior eye, and pain will be the only symptom. Associated inflammation of the orbit may result in proptosis (exophthalmos) and impaired ocular motility due to myositis of the ocular muscles. Intraocular findings may include exudative retinal detachment and/or choroid detachment. Macular and optic disk edema are frequently present.
The reddening in scleritis is due to injection
of the deeper vascular plexus on the sclera and to injection of the episclera.
Inspecting the eye in daylight will best reveal the layer of maximum injection.
Differential diagnosis:
Conjunctivitis and episcleritis (see that
section).
Treatment:
Anterior non-necrotizing scleritis.Topical or systemicnonsteroidalanti-inflammatory
therapy.
Anterior necrotizing scleritis with inflammation.Systemicsteroidtherapy
isusually required to control pain. If corticosteroids do not help or are not
tolerated, immunosuppressive agents may be used.
Anterior necrotizing scleritis without inflammation
(scleromalacia per-forans).As no effective treatment is available, grafts of preserved
sclera orlyophilized dura may be required to preserve the globe if the course
of the disorder is fulminant.
Posterior scleritis.Treatment is the same as for anterior necrotizing scleritiswith
inflammation.
Related Topics