Chapter: Psychiatric Mental Health Nursing : Therapeutic Relationships
Roles of the Nurse in a Therapeutic Relationship
ROLES OF THE NURSE IN A
THERAPEUTIC RELATIONSHIP
As when working with clients in any other nursing setting, the
psychiatric nurse uses various roles to provide needed care to the client. The
nurse understands the importance of assuming the appropriate role for the work
that he or she is doing with the client.
Teacher
The teacher role is inherent in most aspects of client care. During
the working phase of the nurse–client relationship, the nurse may teach the
client new methods of coping and solving problems. He or she may instruct about
themedication regimen and available community resources. To be a good teacher,
the nurse must feel confident about the knowledge he or she has and must know
the limita-tions of that knowledge base. The nurse should be familiar with the
resources in the health-care setting and commu-nity and on the Internet, which
can provide needed infor-mation for clients. The nurse must be honest about
what information he or she can provide and when and where to refer clients for
further information. This behavior and honesty build trust in clients.
Caregiver
The primary caregiving role in mental health settings is the
implementation of the therapeutic relationship to build trust, explore
feelings, assist the client in problem-solving, and help the client meet
psychosocial needs. If the client also requires physical nursing care, the
nurse may need to explain to the client the need for touch while per-forming
physical care. Some clients may confuse physical care with intimacy and sexual
interest, which can erode the therapeutic relationship. The nurse must consider
the relationship boundaries and parameters that have been established and must
repeat the goals that were established together at the beginning of the
relationship.
Advocate
In the advocate role, the nurse informs the client and then
supports him or her in whatever decision he or she makes (Edd, Fox, &
Burns, 2005). In psychiatric–mental health nursing, advocacy is a bit different
from medical-surgical set-tings because of the nature of the client’s illness.
For example, the nurse cannot support a client’s decision to hurt himself or
herself or another person. Advocacy
is the process of acting on the client’s behalf when he or she cannot do so.
This includes ensuring privacy and dignity, promoting informed consent,
preventing unnecessary examinations and proce-dures, accessing needed services
and benefits, and ensuringsafety from abuse and exploitation by a health
professional or authority figure. For example, if a physician begins to
exam-ine a client without closing the curtains and the nurse steps in and
properly drapes the client and closes the curtains, the nurse has just acted as
the client’s advocate.
Being an advocate has risks. In the previous example, the physician
may be embarrassed and angry and make a comment to the nurse. The nurse needs
to stay focused on the appropriateness of his or her behavior and not be
intimidated.
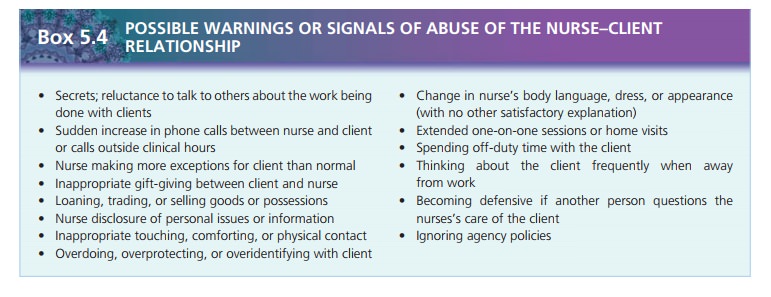
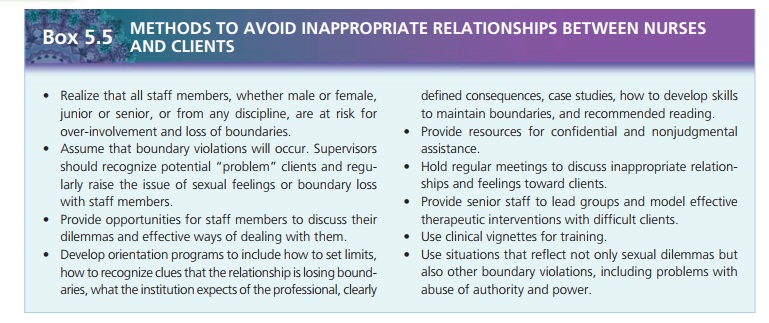
The role of advocate also requires the nurse to be obser-vant of
other health-care professionals. At times, staff mem-bers may be reluctant to
see what is happening or become involved when a colleague violates the
boundaries of a pro-fessional relationship. Nurses must take action by talking
to the colleague or a supervisor when they observe boundary violations. State
nurse practice acts include the nurse’s legal responsibility to report boundary
violations and unethical conduct on the part of other health-care providers.
There is debate about the role of nurse as advocate. There are
times when the nurse does not advocate for the client’s autonomy or right to
self-determination, such as by supporting involuntary hospitalization for a
suicidal client. At these times, acting in the client’s best interest (keeping
the client safe) is in direct opposition to the cli-ent’s wishes. Some critics
view this as paternalism and interference with the true role of advocacy. In
addition, they do not see advocacy as a role exclusive to nursing but also
relevant to the domains of physicians, social workers, and other health-care
professionals.
Parent Surrogate
When a client exhibits child-like behavior or when a nurse is
required to provide personal care such as feeding or bathing, the nurse may be
tempted to assume the parental role as evidenced in choice of words and
nonverbal com-munication. The nurse may begin to sound authoritative with an
attitude of “I know what’s best for you.” Often, the client responds by acting
more child-like and stubborn. Neither party realizes they have fallen from
adult–adult communication to parent–child communication. It is easy for the
client to view the nurse in such circumstances as a parent surrogate. In such
situations, the nurse must be clear and firm and set limits or reiterate the
previously set limits. By retaining an open, easygoing, nonjudgmental attitude,
the nurse can continue to nurture the client while establishing boundaries. The
nurse must ensure the rela-tionship remains therapeutic and does not become
social or intimate.
Related Topics