Chapter: Psychiatric Mental Health Nursing : Therapeutic Relationships
Establishing the Therapeutic Relationship
ESTABLISHING THE THERAPEUTIC
RELATIONSHIP
The nurse who has self-confidence rooted in self- awareness is ready
to establish appropriate therapeutic relationships with clients. Because
personal growth is ongoing over one’s lifetime, the nurse cannot expect to have
complete self-knowledge. Awareness of his or her strengths and limita-tions at
any particular moment, however, is a good start.
Phases
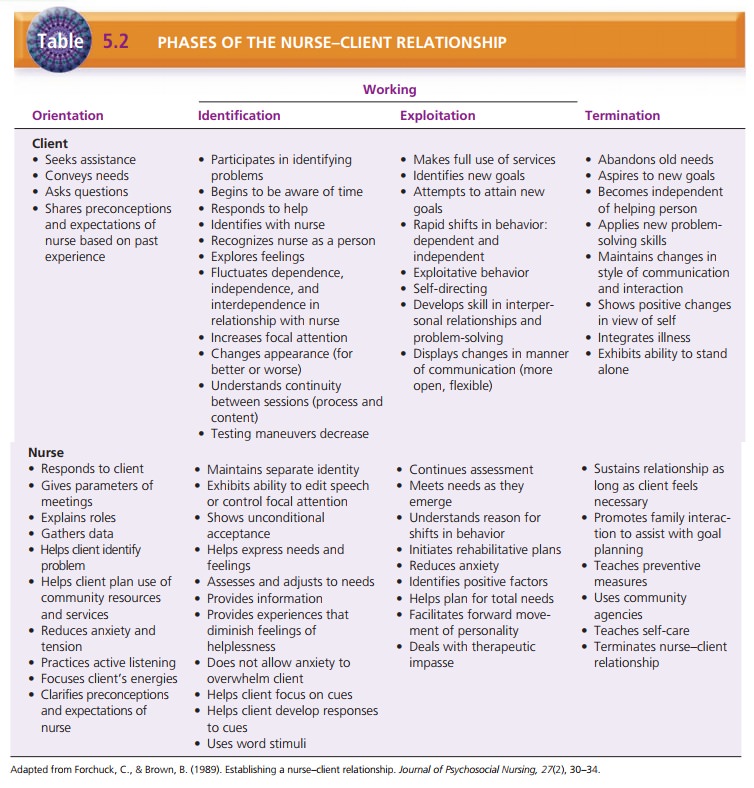
Peplau studied and wrote about the interpersonal pro-cesses and the
phases of the nurse–client relationship for 35 years. Her work provides the
nursing profession with a model that can be used to understand and document
prog-ress with interpersonal interactions. Peplau’s model (1952) has three
phases: orientation, working, and resolution or termination (Table 5.2). In
real life, these phases are not that clear-cut; they overlap and interlock.
Orientation
The orientation phase
begins when the nurse and client meet and ends when the client begins to
identify problems to examine. During the orientation phase, the nurse
estab-lishes roles, the purpose of meeting, and the parameters of subsequent
meetings; identifies the client’s problems; and clarifies expectations.
Before meeting the client, the nurse has important work to do. The
nurse reads background materials available on the client, becomes familiar with
any medications the cli-ent is taking, gathers necessary paperwork, and
arranges for a quiet, private, and comfortable setting. This is the time for
self-assessment. The nurse should consider his or her personal strengths and
limitations in working with this client. Are there any areas that might signal
difficulty because of past experiences? For example, if this client is a spouse
batterer and the nurse’s father was also one, the nurse needs to consider the
situation: How does it make him or her feel? What memories does it prompt, and
can he or she work with the client without these memories interfering? The
nurse must examine preconceptions about the client and ensure that he or she
can put them aside and get to know the real person. The nurse must come to each
client without preconceptions or prejudices. It may be useful for the nurse to
discuss all potential prob-lem areas with the instructor.
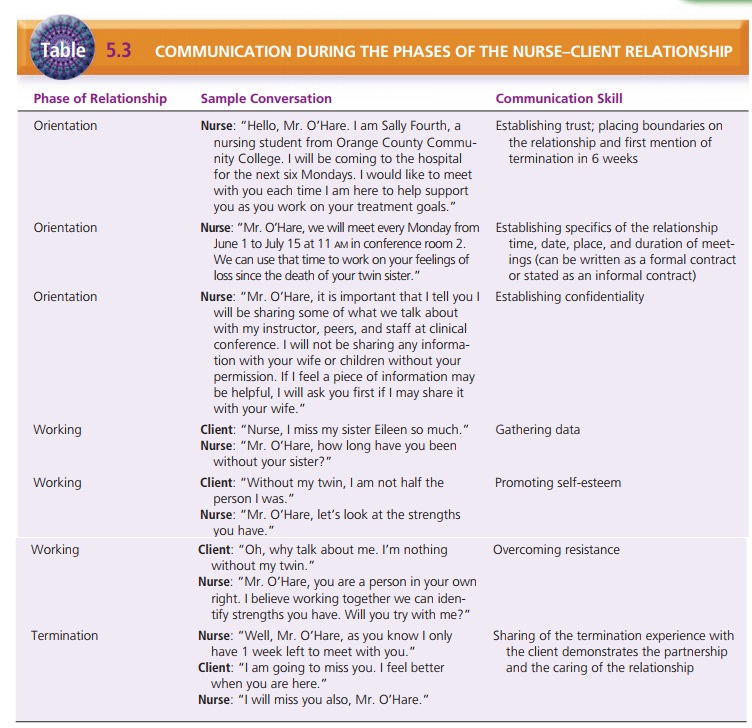
During the orientation phase, the nurse begins to build trust with
the client. It is the nurse’s responsibility to establish a therapeutic
environment that fosters trust and understanding (Table 5.3). The nurse should
share appropriate information about himself or herself at this time, including
name, reason for being on the unit, and level of schooling: For example,
“Hello, James. My name is Miss Ames and I will be your nurse for the next six
Tuesdays. I am a senior nursing student at the University of Mississippi.”
The nurse needs to listen closely to the client’s history,
perceptions, and misconceptions. He or she needs to con-vey empathy and
understanding. If the relationship gets off to a positive start, it is more
likely to succeed and to meet established goals.
At the first meeting, the client may be distrustful if pre-vious
relationships with nurses have been unsatisfactory. The client may use rambling
speech, act out, or exaggerate episodes as ploys to avoid discussing the real
problems. It may take several sessions until the client believes that he or she
can trust the nurse.
Nurse–Client Contracts. Although many clients have
had prior experiences in the mental health system,
the nurse
must once again outline the responsibilities of the nurse and the
client. At the outset, both nurse and client should agree on these
responsibilities in an informal or verbal contract. In some instances, a formal
or written contract may be appropriate; examples include if a written contract
has been necessary in the past with the client or if the cli-ent “forgets” the
agreed-on verbal contract.
The contract should state the following:
·
Time, place, and length of sessions
·
When sessions will terminate
·
Who will be involved in the treatment plan (family members or
health team members)
·
Client responsibilities (arrive on time and end on time)
·
Nurse’s responsibilities (arrive on time, end on time, maintain
confidentiality at all times, evaluate progress with client, and document
sessions).
Confidentiality. Confidentiality means respecting the client’s right to keep
private any information about his or her mental and physical health and related
care. It means allowing only those dealing with the client’s care to have
access to the information that the client divulges. Only under precisely
defined conditions can third parties have access to this information; for
example, in many states the law requires that staff report suspected child and
elder abuse.
Adult clients can decide which family members, if any, may be
involved in treatment and may have access to clinical information. Ideally, the
people close to the client and responsible for his or her care are involved.
The cli-ent must decide, however, who will be included. For the client to feel
safe, boundaries must be clear. The nurse must clearly state information about
who will have access to client assessment data and progress evaluations. He or
she should tell the client that members of the mental health team share
appropriate information among them-selves to provide consistent care and that
only with the client’s permission will they include a family member. If the
client has an appointed guardian, that person can review client information and
make treatment decisions that are in the client’s best interest. For a child,
the parent or appointed guardian is allowed access to information and can make
treatment decisions as outlined by the health-care team.
The nurse must be alert if a client asks him or her to keep a
secret because this information may relate to the client’s harming himself or
herself or others. The nurse must avoid any promises to keep secrets. If the
nurse has promised not to tell before hearing the message, he or she could be
jeopardizing the client’s trust. In most cases, even when the nurse refuses to
agree to keep information secret, the client continues to relate issues anyway.
The following is an example of a good response to a client who is suicidal but
requests secrecy:
Client: “I am going to jump off the 14th floor of my apartment building tonight, but please don’t tell
anyone.”
Nurse: “I cannot keep such a promise, espe-cially if it involves your
safety. I sense you arefeeling frightened. The staff and I will help you stay
safe.”
The Tarasoff vs. Regents of
the University of California (1976) decision releases professionals from
privileged communication with their clients should a client make a homicidal
threat. The decision requires the nurse to notify intended victims and police
of such a threat. In this cir-cumstance, the nurse must report the homicidal
threat tothe nursing supervisor and attending physician so that both the police
and the intended victim can be notified. This is called a duty to warn.
The nurse documents the client’s problems with planned
interventions. The client must understand that the nurse will collect data about
him or her that helps in making a diagnosis, planning health care (including
medications), and protecting the client’s civil rights. The client needs to
know the limits of confidentiality in nurse–client interac-tions and how the
nurse will use and share this informa-tion with professionals involved in
client care.
Self-Disclosure. Self-disclosure means revealing per-sonal information such as
biographical information and personal ideas, thoughts, and feelings about
oneself to cli-ents. Traditionally, conventional wisdom held that nurses should
share only their name and give a general idea about their residence, such as “I
live in Ocean County.” Now, however, it is believed that some purposeful,
well-planned, self-disclosure can improve rapport between the nurse and the
client. The nurse can use self-disclosure to convey support, educate clients,
and demonstrate that a client’s anxiety is normal and that many people deal
with stress and problems in their lives.
Self-disclosure may help the client feel more comfort-able and more
willing to share thoughts and feelings, or help the client gain insight into
his or her situation. When using self-disclosure, the nurse must also consider
cultural factors. Some clients may deem self-disclosure inappropriate or too personal,
causing the client discom-fort. Disclosing personal information to a client can
be harmful and inappropriate, so it must be planned and considered thoughtfully
in advance. Spontaneously self-disclosing personal information can have
negative results. For example, when working with a client whose parents are
getting a divorce, the nurse says, “My parents got a divorce when I was 12 and
it was a horrible time for me.” The nurse has shifted the focus away from the
client and has given the client the idea that this experience will be horrible
for the client. Although the nurse may have meant to communicate empathy, the
result can be quite the opposite.
Working
The working phase of the
nurse–client relationship is usually divided into two subphases: During problem identification, the client identifies the issues or concerns causing problems. During exploitation, the nurse guides the
client to examine feelings and responses and to develop better coping skills
and a more positive self-image; this encourages behavior change and develops
independence. (Note that Peplau’s use of the word exploi-tation had a very different meaning than current usage, which involves unfairly using or taking
advantage of a person or situation. For that reason, this phase is better![]()
![]() conceptualized as intense exploration and
elaboration on earlier themes that the client discussed.) The trust
estab-lished between nurse and client at this point allows them to examine the
problems and to work on them within the security of the relationship. The
client must believe that the nurse will not turn away or be upset when the
client reveals experiences, issues, behaviors, and problems. Sometimes the
client will use outrageous stories or act-ing-out behaviors to test the nurse.
Testing behavior chal-lenges the nurse to stay focused and not to react or to
be distracted. Often when the client becomes uncomfortable because he or she is
getting too close to the truth, he or she will use testing behaviors to avoid
the subject. The nurse may respond by saying, “It seems as if we have hit an
uncomfortable spot for you. Would you like to let it go for now?” This
statement focuses on the issue at hand and diverts attention from the testing
behavior.
conceptualized as intense exploration and
elaboration on earlier themes that the client discussed.) The trust
estab-lished between nurse and client at this point allows them to examine the
problems and to work on them within the security of the relationship. The
client must believe that the nurse will not turn away or be upset when the
client reveals experiences, issues, behaviors, and problems. Sometimes the
client will use outrageous stories or act-ing-out behaviors to test the nurse.
Testing behavior chal-lenges the nurse to stay focused and not to react or to
be distracted. Often when the client becomes uncomfortable because he or she is
getting too close to the truth, he or she will use testing behaviors to avoid
the subject. The nurse may respond by saying, “It seems as if we have hit an
uncomfortable spot for you. Would you like to let it go for now?” This
statement focuses on the issue at hand and diverts attention from the testing
behavior.
The nurse must remember that it is the client who examines and
explores problem situations and relation-ships. The nurse must be nonjudgmental
and refrain from giving advice; the nurse should allow the client to analyze
situations. The nurse can guide the client to observe pat-terns of behavior and
whether or not the expected response occurs. For example, a client who suffers
from depression complains to the nurse about the lack of concern her chil-dren
show her. With the assistance and guidance of the nurse, the client can explore
how she communicates with her children and may discover that her communication
involves complaining and criticizing. The nurse can then help the client
explore more effective ways of communi-cating in the future. The specific tasks
of the working phase include the following:
·
Maintaining the relationship
·
Gathering more data
·
Exploring perceptions of reality
·
Developing positive coping mechanisms
·
Promoting a positive self-concept
·
Encouraging verbalization of feelings
·
Facilitating behavior change
·
Working through resistance
·
Evaluating progress and redefining goals as appropriate
·
Providing opportunities for the client to practice new behaviors
·
Promoting independence.
As the nurse and client work together, it is common for the client
unconsciously to transfer to the nurse feelings he or she has for significant
others. This is called transfer-ence.
For example, if the client has had negative experi-ences with authority
figures, such as a parent or teachers or principals, he or she may display
similar reactions of negativity and resistance to the nurse, who also is viewed
as an authority. A similar process can occur when the nurse responds to the
client based on personal unconscious needs and conflicts; this is called countertransference. For example, if
the nurse is the youngest in her family and often felt as if no one listened to
her when she was a child, she may respond with anger to a client who does not
listen or resists her help. Again, self-awareness is important so that the
nurse can identify when transference and counter-transference might occur. By
being aware of such “hot spots,” the nurse has a better chance of responding
appro-priately rather than letting old unresolved conflicts inter-fere with the
relationship.
Termination
The termination or
resolution phase is the final stage in the nurse–client relationship. It
begins when the prob-lems are resolved, and it ends when the relationship is
ended. Both nurse and client usually have feelings about ending the
relationship; the client especially may feel the termination as an impending
loss. Often clients try to avoid termination by acting angry or as if the
problem has not been resolved. The nurse can acknowledge the client’s angry
feelings and assure the client that this response is normal to ending a
relationship. If the client tries to reopen and discuss old resolved issues,
the nurse must avoid feeling as if the sessions were unsuccessful; instead, he
or she should identify the client’s stalling maneuvers and refocus the client
on newly learned behaviors and skills to handle the problem. It is appropriate
to tell the client that the nurse enjoyed the time spent with the cli-ent and
will remember him or her, but it is inappropriate for the nurse to agree to see
the client outside the thera-peutic relationship.
Related Topics