Chapter: Medicine Study Notes : Surgical and Fluid Management
Replacement fluids
Replacement fluids
Signs of extracellular fluid depletion
·
Symptoms: oliguria (min 0.5
ml/kg/hr), thirst, tachycardia, dry tongue, weakness, confusion
·
Signs: weight change, ¯tissue
turgor, postural hypotension, cool peripheries, dry axilla and mucous
membranes, ¯JVP
·
Common in surgical patients due
to: vomiting, ileus, stomal losses, etc. Not always naso-gastric losses.
Frusemide is a flogging offence! It‟s due to intravascular hypovolaemia
· Investigations:
o Bloods: Hb, Urea/Creatinine, Na/K
o Urine Na
o Maybe ABG for acid/base balance
·
Replace deficit quickly over 30
minutes – 1 ½ hours, not by increasing hourly rate
·
Give boluses of 200-250 mls
N/saline, Hartmanns or plasma expander
·
Take care in older patients/CHD:
don‟t tolerate large Na loads (® pulmonary oedema)
·
If on IPPV, this pushes up
intra-thoracic pressure to 10 – 15 cm H2O (0 – 5 cm H2O is normal), so when
using central venous pressure need to adjust for this before determining
whether hypovolaemic
Depletion in children
·
Can be rapid and profound. Described as:
o Mild: loss of 4 – 5 % body mass.
History of diarrhoea/vomiting but few signs
o Moderate: loss of 6 – 9 % body mass.
Sunken eyes & fontanelle.
Urine output < 0.5 mls/kg/hour
o Severe: 10% loss of body mass.
Very ill. Hypotension and rapid
weak pulse
Types of Replacement Fluids
·
Crystalloids: isotonic, short
intravascular T½ . For replacement of extra-cellular loss. To replace blood
give 3 times blood loss
o 0.9 % saline: 154 mmol/L NaCl (isotonic)
o Hartmanns and Lactated Ringers: electrolyte mixture similar to plasma
o Excessive replacement of plasma losses acutely with saline may ®
hyperchloraemic acidosis
·
Dextrose containing solutions:
not for replacing blood loss (hypertonic). For treatment of water loss or when
sodium restrictions are present:
o Barts: 4% dextrose/0.18% saline – 30 mmol/L NaCl + 168 Kcal/L
o 5% dextrose: 200 Kcal/L (calories and water only)
· Synthetic Colloids: isotonic, long intravascular T½, for blood volume replacement. More readily available than blood and no infection risk, don‟t require cross matching. Give 1:1 ratio with blood lost. If > 1 L required, consider albumin and/or blood. Kidneys take time to excrete, so watch for fluid overload, especially in renal impairment and kids
o Haemaccel: polygeline (degraded gelatine) plus electrolytes (145 mmol/L NaCl + 5.1 mmol/L K + 6.25 mmol./L Ca). T½ = 4 hours, hypersensitivity rare
o Dextran 40, 70: dextran with molecular weight 40K (T½ = 2 – 4 hours) or
70K (T½ = 6 hours), hypersensitivity reactions, impairs coagulation and cross
match
o Hetastarch (Hespan), Pentaspan: starch solution, MR = 70K, T½ = 17
hours, hypersensitivity rare
·
Blood products: reserved for >
20% blood loss or continuing bleeding or Hb acutely < 70 g/L
·
If fluids not hypo-osmotic
compared with blood, then red cell would swell ®
haemolysis
·
Warm fluids, especially if
refrigerated. Haemaccel and crystalloids
can be microwaved
Child Requirements
·
Maintenance fluid: 4% dextrose +
0.18% saline + 20 mmol KCl/L at:
§ Per hour Per day
o First 10 kg 4 mls/kg 100 mls/kg
o Second 10
kgs 2 mls/kg 50 mls/kg
o All
subsequent kgs 1 ml/kg 25 mls/kg
· Losses (e.g. nasogastric tube, fever, diarrhoea) replaced with an equal volume of 0.45% NaCl + 20 mmol KCl/L. Give as boluses of 20 ml/kg over 15 – 30 mins. Losses decrease with renal failure
·
Admit or observe in a short stay
facility for several hours
·
Don‟t use homemade solutions –
use Gastrolyte
· Orally, of by NG tube if necessary:
o Replace calculated losses over 6 hours (don‟t worry about maintenance
requirements). Hourly observations and reassess and reweigh after 6 hours
o Give the remainder of the daily fluid maintenance over the next 18 hours
·
Resume breast feeding as soon as
rehydration is complete or sooner if this takes longer than 6-hours
· If after 4 – 6 hours the child remains dehydrated, then IV
Adult requirements
·
Adult daily requirements:
o 2.5 - 3 litres of fluid
o 100 mmol Na (60 mmol/day in elderly)
o 60 mmol of K+ (max of 10 mmol per hour)
· Can be given as:
o 2.5 – 3 litres of dextrose/saline (=0.18% saline + 4% dextrose) per day
with 20 mmol/L KCl in each bag, or
o 2 litres of 5% dextrose and 500 mls of saline
o Run in at 50 – 100 mls per hour (NB, smaller daily requirements for a
small person)
o If concerned about heart failure/pulmonary oedema than monitor saturation
·
Intraoperative fluid replacement:
o Oral intake withheld before surgery
o In major surgery, half the estimated 24 hour maintenance requirement should be given initially (600 – 1000 ml saline), followed by maintenance requirements plus loses
o K is usually excluded for first few post-operative days: due to
liberation from cells
o Excess use of low Na fluids post-operatively may cause hyponatraemia
given ADH
Abdominal losses
·
GIT has huge internal economy of
fluid secretion & absorption
· Losses through surgical intervention (stoma, leaking viscous, etc) replaced with iv solution of similar composition

·
Saliva 1500
·
Gastric 1500
·
Pancreatic 700
·
Bilary 500
·
Jejunostomy 2-3000
·
Ileostomy 500
·
Colostomy 300
·
Diarrhoea 0.5
– 15,000 (Normal ileum delivers 1200 – 1500 per day)
·
Diarrhoea and Vomiting
o Leads to dehydration, hyponatraemia, hypokalaemia, hypochloraemia
o Replace ½ calculated losses in first 24 hours with saline plus
potassium. Maximum rate of potassium replacement is 20 mmol/hr
Burns
·
Burns ® rapid
loss ® secondary organ damage (e.g. renal)
·
Give 2-4 mls/kg * %burned area of
Hartmanns: half over first 8 hours, rest over next 16, in addition to maintenance requirements. Consider blood transfusion
Monitoring adequacy of Fluid Replacement
·
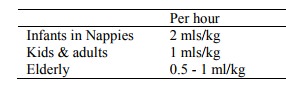
Monitor pulse, BP, respiratory
rate and urine output (i.e. put in catheter):
·
Na to K ratio in urine should be
> 1. If < 1 then body frantically
reabsorbing Na Þ not in balance
Postoperative Hyponatraemia
· Normal value of Na: 135 – 145 mmol/L
· Hyponatraemia is not a diagnosis – it is found in diverse conditions. Body Na may be low, normal or high. Relative water retention is a common factor
· Condition and treatment can be hazardous. If correct too fast then pontine demyelination
· Treatment must be slow and monitored closely. Treatment can range from water restriction or diuresis to sodium restriction or normal saline. Need to know underlying cause
· Don‟t use hypotonic fluids post-op unless Na is high. Eg dextrose saline – glucose absorbed very quickly post surgery ® hypotonic
Symptoms:
·
The big boogie is underlying
cerebral oedema. Bigger problem if abrupt onset. Rapid correction can cause
central pontine melanosis
·
Symptoms don‟t correlate well
with [Na]
·
Early: anorexia, headache,
nausea, vomiting, muscle cramps, weakness
·
Advanced: mutism, dysarthria, impaired response to
verbal or painful stimuli, bizarre behaviour, hallucinations, asterixis,
incontinence, respiratory insufficiency, spastic quadriparesis in 90%
·
Far advanced: (too late to do much) decorticate or
decerebrate posturing, bradycardia, hypo or hypertension, dilated pupils,
seizures, respiratory arrest, coma, polyuria (central diabetes insipidous)
· Should always be a differential in post-operative coma
Related Topics