Chapter: Medicine Study Notes : Surgical and Fluid Management
Blood Products
Blood Products
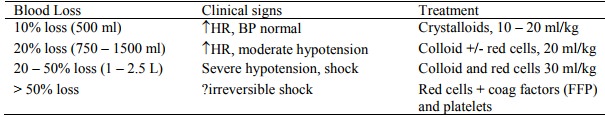
Blood loss
·
Giving blood isn‟t based on how
much they‟ve lost, but on Hb measurement and pre-existing cardiac/respiratory
disease. A normal person could survive an Hb of 50 if volume was adequate
(below this CO falls dramatically). But a sick, old person can‟t use CO to
compensate, so CO starts to drop below 100
Blood Component Therapy
·
Modern transfusion therapy is
blood component therapy
·
Blood components are used to:
o Correct intravascular volume (usually non-human products e.g.
crystalloids)
o Correct O2 transport deficiency
o Correct bleeding disorders
· Blood components available:
o Red cells: one unit is the red cells from one unit of donated blood (450 ml). Hb increases by 10 g/L per unit transfused. Red cell transfusions – transfuse at 1 unit per 2 – 4 hours (if cardiovascularly healthy then 2 hours, if older then 4 hours as you don‟t‟ want to go too fast otherwise volume overload)
o Platelet concentrates: Prophylactic platelet transfusions – 10 g/L
pretty good maintenance level in leukaemia.
o Fresh frozen plasma: 250 ml will
provide approx 8% of an adult‟s circulating clotting factors
o Cryoprecipitate: source of fibrinogen for DIC
o VIII & IX concentrates
o To separate these: centrifuge – take off plasma first, then platelets,
then RBCs
·
Decision sequence:
o What factor is deficient?
o Is the deficiency physiologically significant (hard to decide. Not the
same as below the normal range, as normal range includes functional reserve)
o What is the appropriate blood product
o What is the correct dose to transfuse
o Has the transfusion worked?
·
When blood is required:
o Type O immediately, type specific in 10 – 20 minutes and full X match in an hour
o If massive transfusion (> 50% loss) use reconstituted red cells and
colloid and consult haematologist re fresh frozen plasma (FFP), platelets and
coagulation factors
o Tests for coagulation during large transfusions should include:
§ Full blood count: baseline Hb and platelet counts before transfusion,
and repeated throughout
§ APPT: intrinsic pathway
§ PT/INR: extrinsic pathway
§ Thrombin time: fibrinogen availability
§ Fibrin degradation products: for DIC
·
Risks:
o Most common reaction to transfusion: febrile ½ an hour later:
§ Due to leukocytes contaminating red cells. If necessary, insert leucocyte filter on line (@$50) ® leucocyte poor red cells
§ Febrile reaction more common if multiple blood transfusions or multiple
children (more antigenically primed)
o ABO incompatibility (eg due to incorrect labelling):
§ Hypotensive, rash, tachycardia
§ Symptoms of major intravascular haemolysis: nausea, vomiting, low back pain (renal reaction to free haemoglobin), feeling very unwell
o If allergic to plasma proteins ® washed red cells
o For immunocompromised: use irradiated red cells to stop leucocytes
grafting into host & then attacking host
o Infection risks (depend on prevalence in population):
§ Bacteria:
·
Yersinia Enterocolitica: is
cryophilic (likes cold) and blood is a great culture medium. Comes from transient
bacteraemia in infected donor.
·
Other bacteria: Brucella abortus,
salmonella, M. Leprae
§ Viruses: HBV, HCV, HIV, HTLV-1, CMV, EBV
§ Parasites: Malaria, Toxoplasma gondii, Trypanosome cruzi
§ Specific risks:
·
HIV infection via transfusion: 1
in 1 – 2 million
·
CJD: no documented case worldwide
(although has been done in animals)
·
HBV: 1 in 200,000
·
HBC: 1 in 80,000
o Complications of massive blood transfusion:
§ Over transfusion ® Fluid overload and pulmonary oedema
§ Coagulation defects: dilutional thrombocytopaenia, ¯factors
V, VII & X, DIC
§ Hypothermia (blood products are stored at 4 C)
§ Hyperkalaemia: K moves out of red cells in storage
§ Acidaemia: stored blood becomes acidotic with age
§ Hypocalcaemia & citrate toxicity ® cardiac depression and alkalosis
§ Hypomagnesaemia
§ Transfusion haemosiderosis (ie iron overload) if on chronic transfusions
(eg thalassaemia)
·
Management of major reaction
(either anaphylaxis/haemolysis or sepsis)
o If worried during the transfusion, stop it
o Call blood bank for advice
o Send back blood + samples from the patient
o Check for errors
·
Strategies to stop transmission
of infection:
o Donor screening – very effective
o Blood screening:
§ But tests not 100% accurate & window periods
§ Move from serologic tests to PCR for viral antigens
Related Topics