Chapter: Essentials of Psychiatry: Psychopathology Across the Life-Cycle
Problems of Early Adulthood
Problems of Early Adulthood
The period between the ages of 20 and 30 years is
commonly referred to as early adulthood.
Early Adult Development
Developmental tasks of early adulthood include achieving emo-tional and financial independence from parents and forming intimate relationships with people outside the family of origin. Stage-specific stressors include leaving home, education and career choice, in some cases service in the armed forces, find-ing and maintaining employment, courtship and marriage, and sexual relations, among others.
Types of Problems
Problems of young adulthood fall mostly into the
categories listed in Table 8.8. By the end of early adulthood, people have
passed through the ages of greatest risk for first onset of the majority of
recognized mental disorders. Comorbidity between disorders becomes the rule
rather than the exception. In a population sur-vey in the USA, 14% of those
evaluated had three or more life-time disorders and accounted for more than 50%
of the mental disorders found, both on a lifetime basis and in the year before
the assessment (Kessler et al.,
1994).
The relationships between comorbid “disorders” are
complex. Whether they indeed represent independent entities with distinctive
etiologies, pathogenetic mechanisms and outcomes, or merely reflect different
ways in which fundamental psychopathological disturbances are manifest over
time, between sexes, or across aspects of psychological functioning remains to
be determined. In some cases, one disorder is clearly antecedent to another.
Examples include disorders of childhood, such as separation anxiety disorder or
conduct disorder, that evolve into adult versions – in these cases, panic
disorder with agoraphobia or antisocial personality disorder, respectively.
Sometimes, as in the case of attention-deficit/hyperactivity disorder, residual
symptoms persist and form the basis for developing problems such as substance
abuse or personality dysfunction. At other times, a second disorder may develop
as a consequence of a primary disorder – in reaction to it or as a
complication. Examples include
major depressive disorder developing after a person
has been incapacitated by panic disorder with agoraphobia, or sedative,
anxiolytic, or alcohol abuse developing because the person attempted to
self-medicate for the condition. Alternatively, disorders appear more or less
contemporaneously and reflect an underlying diathesis or vulnerability. Thus,
patients present with several disorders, all suggestive of a problem of
generalized impulsivity, such as bulimia nervosa, a substance use disorder and
an impulse control disorder (e.g., kleptomania). Personality disorders often
develop in the context of underlying traits affecting specific capacities such
as impulse control or interpersonal relatedness, as dysfunction becomes
widespread.
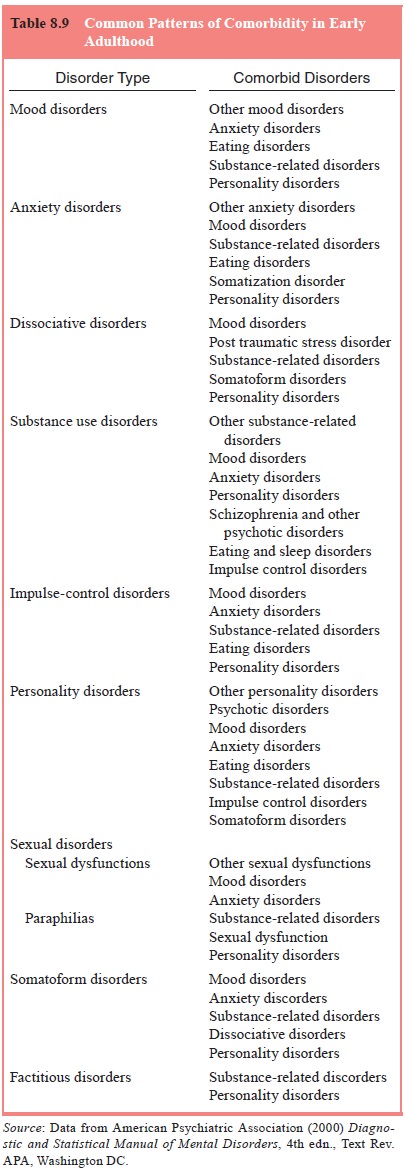
Table 8.9 summarizes patterns of comorbid mental
disor-ders in early adulthood.
Emotional Problems
Although disturbances in mood can occur at any age,
the peak ages of onset of mood disorders are probably in the twenties. Mood
disturbances may be acute and episodic or insidious and chronic. They may be
relatively mild or severe and may be ac-companied by psychotic features or
suicidal behavior. The most common mood disorders are major depressive
disorder, dys-thymic disorder, bipolar disorder and cyclothymic disorder.
Although several anxiety disorders have their onset
most often in childhood or adolescence, as previously described, others have
increased risk for onset in early adult life. In particular, many cases of
acrophobia (fear of heights) and situational phobias, such as of elevators,
flying, or closed places, develop in early adulthood (American Psychiatric
Association, 2000). There is a rise in the rate of panic disorder in women in
early and middle adult life (Regier et
al., 1988). Obsessive–compulsive disorder has a later age at onset in women
than in men, during the twenties rather than the teens. Acute stress disorder
and PTSD can occur at any age but are prevalent in young adults.
Disorders such as panic disorder, other specific
phobias, social phobia and generalized anxiety disorder, which are more likely
to begin in childhood or adolescence, may persist or recur during early adult
life.
The severity, duration and proximity of a person’s
expo-sure to a traumatic event influence the risk of developing either an acute
stress disorder or PTSD (March, 1993). Acute stress reactions which do not
resolve (Classen et al., 1998),
peritrau-matic dissociation (Shalev et
al., 1996) or emotional numbing in response to the stressor (Epstein et al., 1998) predict later PTSD. Social
support, family history, childhood experiences, personal-ity variables and
preexisting mental disorders also affect risk. Men and women appear equally
vulnerable. Dissociative dis-turbances may occur in the absence of
reexperiencing or avoid-ance symptoms, often in response to severe stress
(Spiegel and Cardena, 1991).
Milder, time-limited reactions to stressors of any
severity may also occur. These are common occurrences that might follow the
breakup of a romantic relationship or the loss of a job. The symptoms may be of
depression, anxiety, or disturbance of conduct. They cause temporarily
decreased performance at school or work or impairment in social relationships.
Provided that the consequences of the stressor are resolved (i.e., the person
resumes dating or obtains a new job), the course of the symptoms and impairment
should be less than 6 months.
Behavior and Adaptive Functioning
Problems with various types of impulsive behaviors and problems with adaptive functioning in general seem particularly prone to become manifest in early adulthood. These problems may de-velop, in part, secondary to the increased stresses of movement away from the protective environments of school and family that characterize the period.
Of major significance in the twenties is the
stabilization of patterns of perceiving, relating to, and thinking about the
envi-ronment and oneself that we call personality. Also, however, in the
twenties, the potential for the development of inflexible and maladaptive
traits that cause distress or interfere with effective social and occupational
functioning may arise. Thus, personality disorders may become evident.
Disturbances in Physical Functioning
Certain disturbances in physical functioning are
likely to become manifest in early adult life. These include disturbances in
sexual functioning, sleep disturbances and some physical complaints that cannot
be fully explained on the basis of a known general medical condition.
Certain disturbances characterized by physical
complaints without known medical etiology have a high incidence rate in early
adulthood. Specifically, conversion reactions, hypochon-driasis and
somatization disorder can be first diagnosed in this age group.
Problems in Reality Testing
Problems in reality testing are reflected in
abnormalities of speech, thinking, perception and self-experience. They are
sug-gestive of psychotic disorders such as schizophrenia. Although
schizophrenia and its counterpart disorder of briefer duration, schizophreniform
disorder, may have an onset in late adoles-cence (or in later adulthood), the
most common age at onset is in early adult life.
Patients who have illness episodes that are
character-ized by major episodes of mood disturbance, either depressed or
manic, accompanied by schizophrenia-like psychotic symp-toms and whose
delusions and hallucinations are also present when mood symptoms are not, are
said to have schizoaffective disorder.
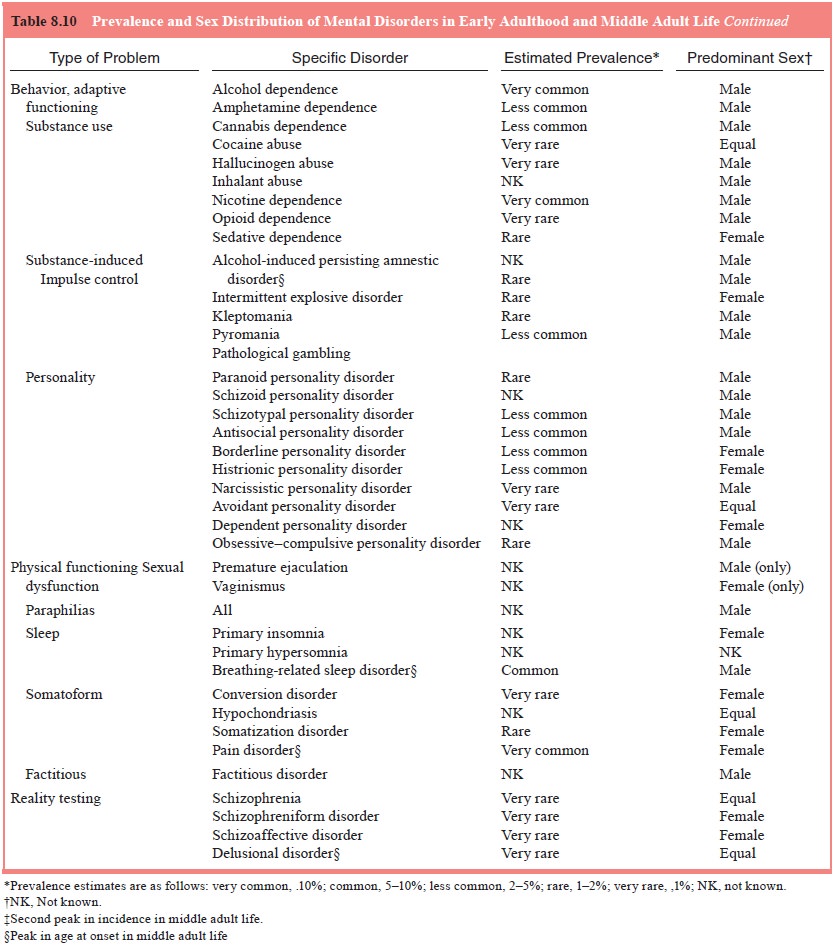
The vast majority of disorders with typical onset
in early adult life persist or recur in middle adult life. Some of these
disorders may also have their initial onset after age 30 years. Table 8.10
summarizes the estimated prevalence and sex distri-bution of mental disorders
of early adulthood.
Related Topics