Chapter: Essentials of Psychiatry: Childhood Disorders: Mental Retardation
Principles of the Use of Psychotropic Drugs in Persons with Mental Retardation
Prerequisites for a Successful
Treatment Program
·
Comprehensive diagnostic understanding
·
Developing goals of treatment
·
Developing treatment priorities
·
Monitoring treatment results
·
Avoidance of indefinite treatment
· Team collaboration
Principles of the Use of
Psychotropic Drugs in Persons with Mental Retardation
This outline is based largely on an excellent
review of Kalachnik and coworkers (1998), Rinck (1998), as well as on the
American Academy of Child and Adolescent Psychiatry (1999), and the Health Care
Financing Administration (1997).
Purpose of Drug Use
These drugs are used to treat a diagnosed mental
disorder toward the goal of maximizing a person’s quality of life. They should
not be used merely to suppress a single, objectionable behavior with-out regard
to the effect on a person’s global adjustment, func-tioning and quality of
life. They cannot be used as punishment, for staff convenience (such as in
understaffed facilities), in lieu of appropriate habilitative program (if such
is unavailable), or in dosages that interfere with such programs and with a
person’s quality of life (Rinck, 1998, p. 52).
Context of Drug Use
These drugs are always used as part of a
comprehensive, treat-ment/habilitation program designed and supervised by an
inter-disciplinary team of which the psychiatric clinician is an integral part.
They should not be prescribed merely in brief “psychop-harmacology
consultation” or “medication review”, in isolation from other aspects of the
treatment.
Prerequisites for Drug Use
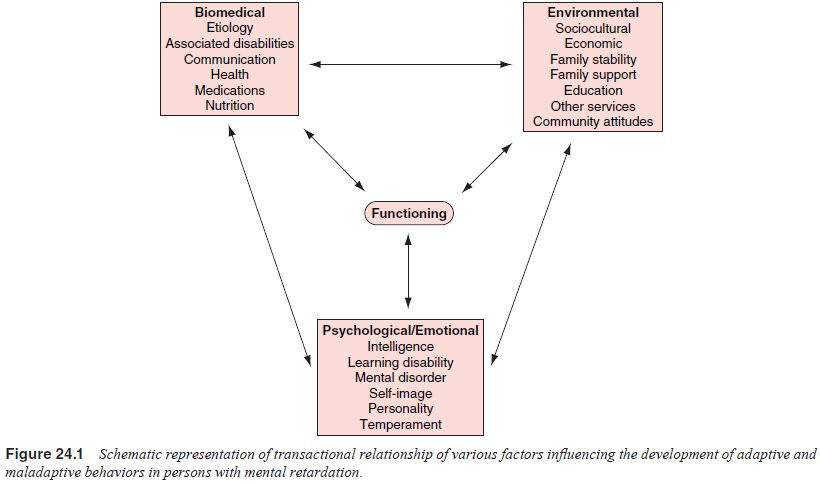
· Comprehensive
psychiatric diagnostic assessment, following the guidelines described earlier
(see also Figure 24.1), and re-sulting in a psychiatric diagnosis.
· Presence
of a comprehensive treatment plan and evidence that less intrusive measures
have not been effective (such as be-havior modification, psychotherapies,
milieu supports, etc.).
· Comprehensive
evaluation to rule out medical conditions that could have caused the presenting
symptoms.
· Existence
of a reliable system to collect behavioral data indi-vidualized to the
particular patient that measures occurrence of symptoms considered an index of
the person’s mental disor-der. This should also provide reliable baseline data
and func-tional analysis of behavior that would assess the influence of
immediate and more remote antecedents and consequences of the patient’s
behaviors and other symptoms.
· Satisfaction
of all relevant regulatory and legal requirements, especially obtaining
informed consent of the patient and/or legal guardian.
Follow-up on Drug Effectiveness
· The
members of the interdisciplinary treatment team should follow the patient’s
progress regularly (at least quarterly), based on changes in individualized
index behaviors, symp-toms, general adjustment, functioning and well-being.
Pres-ence of side effects and their findings should be communi-cated among the
members of the team. Behavioral changes should be documented by reliable data.
The follow-up should include a direct psychiatric interview and/or observation
of the patient. The implementation of all aspects of the treatment program and
not just the medications should be monitored and adjusted as needed to ensure
that medications are not used in lieu of, but concurrently with, a habilitation
program.
·
The medication should be tried at an effective dose
for an ad-equate period of time. If there is no clear evidence of
effec-tiveness it should be discontinued appropriately. It should be kept in
mind that “ups and downs” are to be expected, such as in reaction to
environmental and physical stressors com-mon in the lives of these patients.
Medication effectivenessshould therefore be judged by a pattern evident over
reason-able period of time and not by one-point observations. For the same
reason, preset dosage schedules linking dosage changes to specific frequencies
of index behaviors are impractical. Multiple medications should be tried only
if there is evidence that a combination is known to be more effective than a
single medication
Dosages and Discontinuation
· The
optimal dosage is the lowest one that achieves the best a compromise between
improving the patient’s quality of life and side effects.
·
A trial of dose reduction and possibly
discontinuation should be regularly considered but should be implemented only
if not contraindicated clinically. Discontinuation, if attempted, should be
gradual, and it may need a prolonged period de-pending on the type of
medication and expected withdrawal effects. It is essential that all involved
caregivers be aware of the possibility of such effects and be ready to deal
with them, rather than demand immediate cessation of the discontinua-tion trial
(this is particularly important with antipsychotics. As-needed (.3.prn) use of
the medication is best avoided to prevent unnecessary use, or limited to clear
situations, such as premedication prior to medical tests if stressful for the
patient.
Monitoring Side Effects
Side effects should be monitored regularly through
direct exami-nation (especially important with nonverbal persons), laboratory
tests, tardive dyskinesia examination, and so on, as appropriate for the
particular drug. Possible drug interactions should be mon-itored as these
patients are often on multiple medications
Related Topics