Definition, Causes, Signs and Symptoms, Stages, Risk Factors, Prevention - Pressure Ulcer | 11th Nursing : Chapter 8 : Nursing Procedures
Chapter: 11th Nursing : Chapter 8 : Nursing Procedures
Pressure Ulcer
Pressure Ulcer
Definition
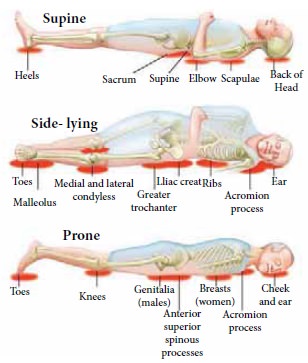
Pressure ulcers, also known as pressure sores, pressure injuries, bedsores, and decubitus ulcers, are localized damage to the skin and/or underlying tissue that usually occur over a bony prominence as a result of pressure, or pressure in combination with shear and/ or friction.
The most common sites
are the skin overlying the sacrum, coccyx, heels or the hips, but other sites
such as the elbows, knees, ankles, back of shoulders, or the back of the
cranium can be affected.
Causes
Pressure ulcers occur
due to pressure applied to soft tissue resulting incompletely or partially
obstructed blood flow to the soft tissue. Shear is also a cause, as it can pull
on blood vessels that feed the skin. Pressure ulcers most commonly develop in
individuals who are not moving about, such as those being bedridden or confined
to a wheelchair.
There are four
mechanisms that contribute to pressure ulcer development:
External (interface) pressure applied over an area of the body, especially
over the bony prominences can result in obstruction of the blood capillaries,
which deprives tissues of oxygen and nutrients, causing ischemia (deficiency of
blood in a particular area), hypoxia (inadequate amount of oxygen available to
the cells), edema, possible onset of osteomyelitis, inflammation, and, finally
necrosis and ulcer formation. Ulcers due to external pressure occur over the
sacrum and coccyx, followed by the trochanter and the calcaneus (heel).
Friction is damaging to the superficial blood vessels directly under the skin. It occurs when two surfaces
rub against each other. The skin over the elbows and can be injured due to
friction.
Shearing is a separation of the skin from underlying tissues. When a patient is partially sitting up in bed,
their skin may stick to the sheet, making them susceptible to shearing in case
underlying tissues move downward with the body toward the foot of the bed.
Moisture is also a common pressure ulcer culprit. Sweat, urine, feces, or excessive wound drainage can
further exacerbate the damage done by pressure, friction, and shear.
Signs and Symptoms
The early signs of
pressure ulcers are
·
Unusual changes in skin color or texture
·
Swelling Tenderness Discomfort
·
Pus-like draining
·
An area of skin that feels cooler or warmer to the touch than
other areas
·
Local oedema
·
Later the area becomes blue purple and mottled
·
Due to continued pressure, the circulation is cut-off, the
gangrene develops and the affected area is sloughed off..
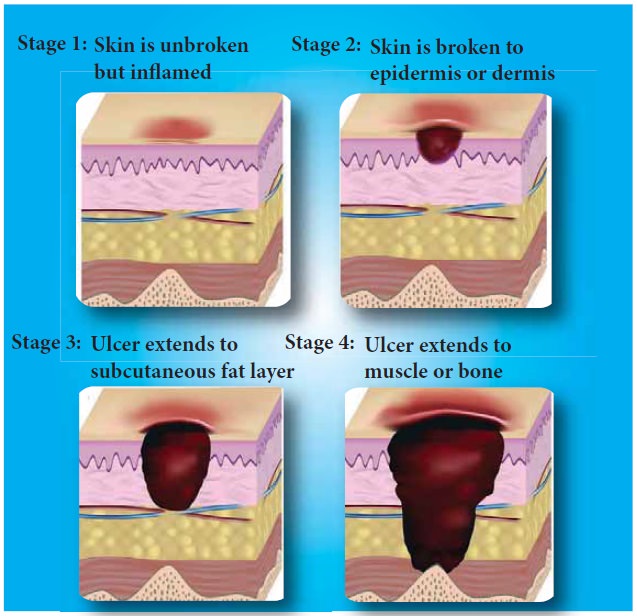
Stages of Pressure Sores
Stage 1
Intact skin with
non-blanch and redness of a localized area usually over a bony prominence.
Stage 2
Partial thickness,
loss of dermis presenting as a shallow open ulcer with a red pink wound bed
without slough may also present as an intact or open/ruptured serum filled
blister. Also presents as a shiny or dry shallow ulcer without slough or
bruising. This stage should not be used to describe skin tears, tape burns,
perinea dermatitis, maceration or excoriation
Stage 3
Full thickness, tissue
loss, subcutaneous fat may be visible but bone, tendon or muscle are not
exposed.
Stage 4
Full thickness tissue
loss with exposed bone, tendon or muscle. Slough or eschar may be present on
some parts of the wound bed.
Unstageable
Full thickness tissue
loss in which actual depth of the ulcer is completely obscured by slough
(yellow, tan, gray, green or brown) and/or eschar (tan, brown or black) in the
wound bed. Until enough slough and/or eschar is removed to expose the base of the
wound, the true depth, and therefore stage, cannot be determined.
Suspected Deep Tissue Injury
A purple or maroon
localized area of discoloured intact skin or blood-filled blister due to damage
of underlying soft tissue from pressure and/or shear. The area may be preceded
by tissue that is painful, firm, mushy, boggy, warmer or cooler as compared to
adjacent tissue.
Areas Prone to Develop Pressure Sore
Risk Factors
Factors that may place
a patient at risk include
·
immobility,
·
diabetes mellitus
·
peripheral vascular disease malnutrition
·
cerebro-vascular accident and hypotension.
·
Other factors are age of 70 years and older,
·
current smoking history, dry skin,
·
low body mass index,
·
urinary and fecal incontinence,
·
physical restraints,
·
malignancy, and history of pressure ulcers.
Prevention
Redistributing pressure:
The most important
care for a person at risk for pressure ulcers and those with bedsores is the
redistribution of pressure so that no pressure is applied to the pressure
ulcer.
Support surfaces
Many support surfaces
redistribute pressure by immersing and/or enveloping the body into the surface.
Some support surfaces, including anti decubitus mattresses and cushions,
contain multiple air chambers that are alternately pumped. Methods to
standardize the products and evaluate the efficacy of these products have only
been developed in recent years.
Nutrition
In addition, adequate
intake of protein and calories is important. vitamin C has been shown to reduce
the risk of pressure ulcers. People with higher intakes of vitamin C have a
lower frequency of bed sores in those who are bedridden than those with lower
intakes.
Treatment
The treatment includes
the use of bed rest, pressure re distributing support surfaces, nutritional
support, repositioning, wound care (e.g. debridement, wound dressings) and
biophysical agents (e.g. electrical stimulation). Reliable scientific evidence
to support the use of many of these interventions, though, is lacking.
The following steps should
be taken:
·
Remove the pressure from the sore by moving the patient or using foam
pads or pillows to prop up parts of the body.
·
Clean the wound: Minor wounds may be gently washed with water and a
mild soap. Open sores need to be cleaned with a saline solution each time the
dressing is changed.
·
Control incontinence as far as possible.
·
Remove dead tissue: A wound does not
heal well if
dead or infected tissue is present, so debridement is
necessary.
·
Apply dressings: These protect the wound and accelerate healing. Some
dressings help prevent infection by dissolving dead tissue.
·
Use oral antibiotic cream: These will help treat an infection.
Debridement
Necrotic tissue should
be removed in most pressure ulcers. The heel is an exception in many cases when
the limb has an inadequate blood supply. Necrotic tissue is an ideal area for
bacterial growth, which has the ability to greatly compromise wound healing.
There are five ways to remove necrotic tissue.
1.
Autolytic debridement is the use of moist dressings to promote autolysis
with the body’s own enzymes and white blood cells.
2.
Biological debridement, or maggot debridement therapy, is the use of
medical maggots to feed on necrotic tissue and therefore clean the wound of
excess bacteria. Although this fell out of favor for many years, in
January2004, the FDA approved maggots as a live medical device.
3.
Chemical debridement, or enzymatic debridement, is the use of prescribed
enzymes that promote the removal of necrotic tissue.
4.
Mechanical debridement, is the use of debriding dressings,
whirlpool or ultrasound for slough in a stable wound
5.
Surgical debridement, or sharp debridement, is the fastest
method, as it allows a surgeon to quickly remove dead tissue.
Dressing
Some guidelines for
dressing are
Condition Cover dressing
None to moderate
exudates - Gauze with tape or composite.
Moderate to heavy
exudates - Foam dressing with tape or composite
Frequent soiling -
Hydrocolloid dressing, film or composite
Fragile skin -Stretch
gauze or stretch net
Related Topics