Chapter: Essentials of Psychiatry: Anxiety Disorders: Traumatic Stress Disorders
Post Traumatic Stress Disorder: Pharmacotherapy
Pharmacotherapy
PTSD may be accompanied by enduring neurochemical and psychophysiological
changes and can lead to substantial im-pairment and distress. Sometimes the
intensity of symptoms is severe enough to preclude the effective use of
trauma-focused psychotherapy. In these situations, the use of medication should
not be delayed unnecessarily. Initial studies showed benefit for the tricyclic
antidepressant and monoamine oxidase inhibitor medications, however, the
selective serotonin reuptake inhibitors (SSRIs) have now replaced these as
first-line agents, based upon evidence from several placebo-controlled trials.
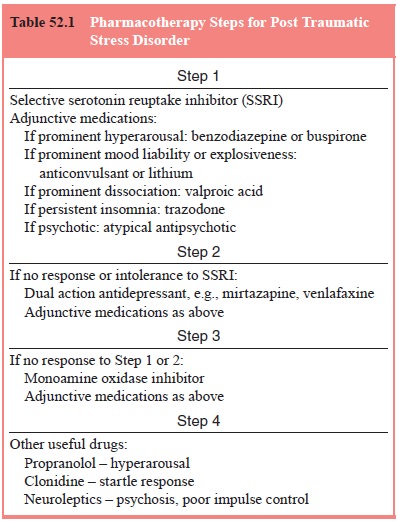
A suggested se-quencing of treatment is outlined in Table 52.1.
Two double-blind clinical trials in more than 100 patients support the
efficacy of amitriptyline and imipramine in com-bat veterans with PTSD (Frank et al., 1988; Davidson et al., 1990). In both studies, the
medication was effective on intrusive PTSD symptoms and, to a weaker extent, on
avoidant symptoms (Table 52.2). Of importance was that clinical efficacy
occurred in patients who did not suffer from depressive illness, suggest-ing
that the effect of tricyclic agents in PTSD is independent o
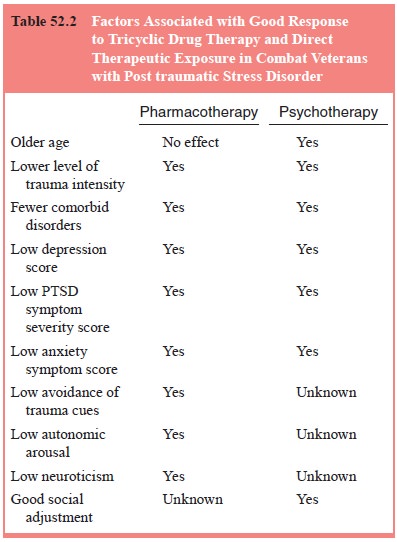
antidepressant properties. In fact response was inversely corre-lated
with baseline depression level.
Phenelzine has been found to be effective in symptom re-duction and that
avoidant symptoms improve to a much greater degree with phenelzine than with
the tricyclic agents. However, the side effects of phenelzine limit its use to
a third- or fourth-line drug to be used only when other, safer medications have
failed to work. Several placebo-controlled trials have shown positive effects
for the SSRI medications, including fluoxetine, sertraline and paroxetine.
Long-term use of sertraline is associated with a substantial reduction in
relapse over a 15-month period. Data support positive effects for SSRI in men
and women and in adults who have survived all major classes of trauma (e.g.,
combat, sexual violence, nonsexual violence and accident). Each of these
medications has broad-spectrum properties across the full symp-tom range of the
disorder as well as improving function and, per-haps, resilience or
stress-coping. They also support the benefit of SSRI in those with and without
comorbid major.
At this
point, the indications for antipsychotic and mood-stabilizing drugs are poorly
defined, but clinical experience suggests that they continue to have a role in
the pharmacologic treatment of PTSD. Antipsychotic medications can be useful in
patients with poor impulse control or in those who manifest features of borderline
personality disorder. Lithium and car-bamazepine can also be useful in such
patients but might benefit individuals who are subject to mood swings and angry
or explo-sive outbursts. The appropriate role for the use of benzodiazepines is
not well-defined. The antiphobic and antiarousal effects of the benzodiazepines
should, in theory, be helpful in PTSD. How-ever, withdrawal from short-acting
benzodiazepines may also introduce an additional set of
problems with intense symptom rebound. In patients who have a propensity to
abuse alcohol and other substances, benzodiazepines are not recommended.
Overall, the antidepressants, mood stabilizers and anticon-vulsants are
the medication groups that are generally considered primary for treating PTSD;
beta-blockers, alpha-2-agonists and anxiolytics have a less clearly defined place. Often,
patients need a combination of drugs but polypharmacy should be utilized in a
carefully planned fashion. Also, since the time course of re-sponse may be
slow, it is advisable to persist with a particular course of action for at
least 8 weeks before deciding that it has been unhelpful. It is possible that
avoidance and numbing symp-toms respond more effectively to SSRI drugs.
Related Topics