Chapter: Essentials of Psychiatry: Anxiety Disorders: Traumatic Stress Disorders
Acute Stress Disorder
Acute Stress Disorder
Definition
It has long been recognized that clinically significant dissocia-tive
states are seen in the immediate aftermath of overwhelm-ing trauma. In
addition, many individuals may experience less clinically severe dissociative
symptoms or alterations of atten-tion and time sense. Because such syndromes,
even when short-lasting, can produce major disruption of everyday activities,
they may require clinical attention. During triage situations after a disaster,
it can be important to recognize this clinical picture, which may require
treatment intervention and which may also be predictive of later PTSD. As a
result of these considerations, a decision was made to include in DSM-IV a new
entity, acute stress disorder (ASD), grouped together with PTSD in the anxiety
disorders section. Essentially, it represents the clinical features of PTSD
along with conspicuous dissociative symptoms, of which at least three must be
present. The possible dissociative symptoms in ASD are a subjective sense of
numbing; detachment or absence of emotional response; reduced awareness of
one’s surroundings; derealization; depersonalization; and dissociative amnesia.
However, there is a lack of empirical evidence for some of the
assumptions inherent in the conceptualization of ASD, and there has been a call
for empirical evidence of acutely trau-matized individuals to address these
assumptions. The current emphasis placed on acute dissociative responses may be
flawed in that there are multiple pathways to PTSD, and most trauma survivors
who display severe acute stress reactions without dis-sociation can develop
PTSD.
Epidemiology
Little is known about the epidemiology of ASD as defined in DSM-IV, but
after events such as rape and criminal assault, the clinical picture of acute
PTSD is found in between 70 and 90% of individuals, although frequency of the
particular dissociative symptoms is unknown. One problem of most postdisaster
surveys is that they evaluate subjects at points several months or years after
the event. This makes any meaningful assessment of acute stress syndromes
difficult. One exception was the self-report-based assessment of morbidity 2
months after an earthquake in Ecuador, which found a 45% rate of caseness
(being a clinical case), with most prominent symptoms being fear, nervousness,
tenseness, worry, insomnia and fatigue (Lima et al., 1989).
Retrospective reports of acute stress symptoms should be interpreted cautiously because of the influence of current symptoms on recall of acute symptoms. In a longitudinal study evaluating report of acute stress symptoms at 1 month and 2 years post trauma, at least one of the four ASD diagnostic clus-ters was recalled inaccurately by 75% of patients (Harvey and Bryant, 2000).
Etiology
Little is known about the etiology of ASD specifically, but it is likely
that many of the same factors that apply to PTSD are rele-vant for ASD that is,
trauma intensity, preexisting psychopathol-ogy, family and genetic
vulnerability, abnormal personality, lack of social supports at the time of the
trauma and physical injury are all likely to increase vulnerability for ASD.
The role of acute arousal in the development of PTSD has been evaluated
in one study (Bryant et al., 2000).
Resting heart rate (HR) and ASD symptoms together were found to account for 36%
of the variance in PTSD prediction. Further, a formula using resting HR
following the trauma exposure (HR . 90 beats/ minute) and the diagnosis of ASD to predict PTSD development
possessed strong sensitivity (88%) and specificity (85%).
Diagnosis and Differential Diagnosis
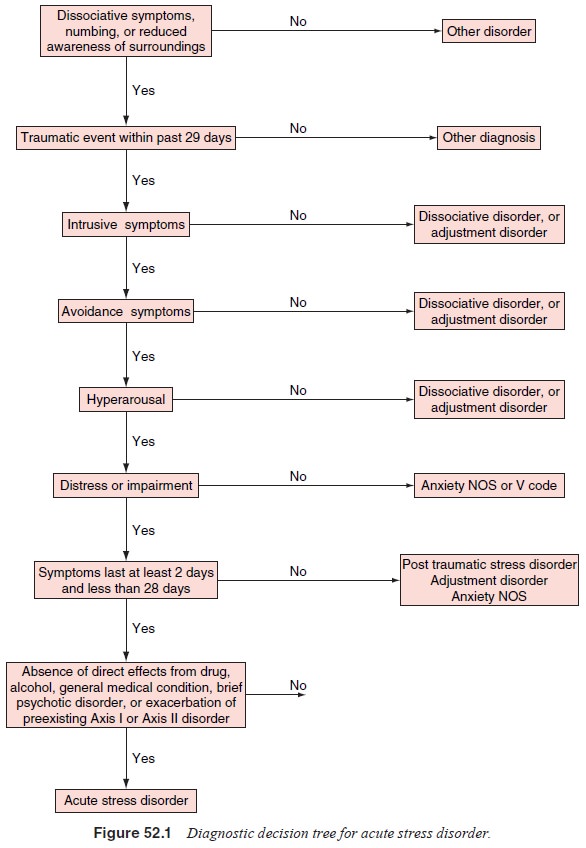
ASD may
need to be distinguished from several related disorders (Figure 52.1). Brief
psychotic disorder may be a more appropriate diagnosis if the predominant
symptoms are psychotic. It is possi-ble that major depressive disorder can
develop post traumaticallyand that there may be some
overlap with ASD, in which case both disorders are appropriately diagnosed.
When ASD-like symptoms are caused by direct physi-ological perturbation,
the symptoms may be more appropri-ately diagnosed with reference to the
etiological agent. Thus, an ASD-like picture that develops secondary to head
injury is more appropriately diagnosed as mental disorder due to a general
medical condition, whereas a clinical picture related to substance use (e.g.,
alcohol intoxication) is appropriately diagnosed as sub-stance-induced
disorder. Substance-related ASD is confined to the period of intoxication or
withdrawal. Head injury-induced ASD needs substantiating by evidence from the
history, physical examination and laboratory testing that the symptoms are a
di-rect physiological consequence of head trauma. Recently, a self-report scale
of ASD has been developed, the Acute Stress Disor-der Scale (ASDS). The scale
has demonstrated good test–retest reliability (r 5 0.94),
and in one sample (bushfire survivors), the ASDS predicted 91% of survivors who
developed PTSD and 93% of those who did not (Bryant et al., 2000).
Because ASD by definition cannot last longer than 1 month, if the
clinical picture persists, a diagnosis of PTSD is ap-propriate. Some increased symptoms
are expected in the great majority of subjects after exposure to major stress.
These remit in most cases and only reach the level of clinical diagnosis if
they are prolonged, exceed a tolerable quality, or interfere with everyday
function. Resolution may be more difficult if there has been previous
psychiatric morbidity, subsequent stress and lack of social support.
Course and Natural History
Although data do not exist on the course and natural history of ASD as
now defined, studies by Kooopman and coworkers (1994) indicated that
dissociative and cognitive symptoms, which are so common in the immediate wake
of trauma, improve sponta-neously with time. However, they also found that the
likelihood of developing PTSD symptoms at 7-month follow-up was more strongly
related to the occurrence of dissociative symptoms than to anxiety symptoms
immediately after exposure to the trauma. However, other studies have
questioned the dissociative criteria as critical for the prediction of later
PTSD.
Treatment
There are six general principles involved in administering any treatment
immediately after trauma. These include principles of brevity, immediacy, centrality,
expectancy, proximity and sim-plicity. That is, treatment of acute trauma is
generally aimed at being brief, provided immediately after the trauma whenever
possible, administered in a centralized and coordinated fashion with the
expectation of the person’s return to normal function and as proximately as
possible to the scene of the trauma, and not directed at any uncovering or
explorative procedures but rather at maintaining a superficial, reintegrating
approach.
People most highly at risk, and therefore perhaps most in need of
treatment, are as follows: survivors with psychiatric dis-orders; traumatically
bereaved people; children, especially when separated from their parents;
individuals who are particularly dependent on psychosocial supports, such as
the elderly, handi-capped and mentally retarded individuals; and traumatized
sur-vivors and body handlers.
Different components of treatment include providing information,
psychological support, crisis intervention and emotional first aid. Providing information
about the trauma is important as it can enable the survivor fully to recognize
and accept all the details of what happened. Information needs to be given in a
way that conveys hope and the possibility that psychological pain and threat of
loss may be coped with. Unrealistic hope needs to be balanced by the provision
of realistic explanations as to what happened. Psychological support helps to
strengthen coping mechanisms and promotes adaptive defenses. The survivor
benefits if he or she recognizes the need to take responsibility for a
successful outcome and is as actively involved with this as possible. Crisis
intervention is often used after disasters and acts of violence or other
serious traumas. It has been described by a number of investigators. Emotional
first aid has been described by Caplan (1984) using the six principles
presented earlier and is used to achieve any of the following: acceptance of
feelings, symptoms, reality and the need for help; recognition of
psychologically distressing issues; identification of available resources;
acceptance of responsibility and absence of blame; cultivation of an optimistic
attitude; and efforts to resume activities of daily life as much as possible.
Civilian trauma survivors with ASD were found to engage in the cognitive
strategies of punishment and worry more than survivors without ASD (Warda and
Bryant, 1998), and cogni-tive–behavioral therapy has been shown to reduce these
strate-gies and increase the use of reappraisal and social control strate-gies.
However, the relation of these findings to the development of PTSD has not yet
been determined.
There is little investigation as to whether early recogni-tion and
effective treatment of acute stress reactions prevent the development of PTSD,
although it is safe to assume that they are likely to have beneficial effects
in this regard. Nonetheless, as was recognized during World War II, rapid and
effective treat-ment of acute combat stress did not always prevent veterans
from developing subsequent chronicity. More recently, an intervention designed
to prevent the development of PTSD and administered in the acute phase,
critical incident stress debriefing, has been found to be ineffective in
preventing the development of PTSD. However, there has been an initial study
with motor vehicle ac-cident survivors that suggested exposure therapy and
exposure therapy with anxiety management training may be effective in
preventing PTSD (Bryant et al.,
1999).
Related Topics