Chapter: Basic & Clinical Pharmacology : Special Aspects of Geriatric Pharmacology
Pharmacologic Changes Associated With Aging
PHARMACOLOGIC CHANGES ASSOCIATED
WITH AGING
In
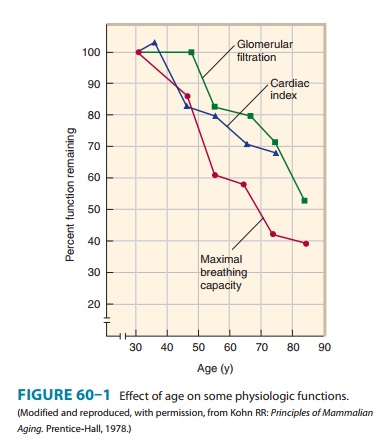
the general population, measurements of functional capacity of most of the
major organ systems show a decline beginning in young adulthood and continuing
throughout life. As shown in Figure 60–1, there is no “middle-age plateau” but
rather a linear decrease beginning no later than age 45. However, these data
reflect the mean and do not apply to every person above a certain age;
approximately one third of healthy subjects have no age-related decrease in,
for example, creatinine clearance up to the age of 75. Thus, the elderly do not
lose specific functions at an accelerated rate compared with young and
middle-aged adults but rather accumulate more deficiencies with the passage of
time. Some of these changes result in altered pharmacokinetics. For the
pharmacologist and the clinician, the most important of these is the decrease
in renal func-tion. Other changes and concurrent diseases may alter the
pharma-codynamic characteristics of particular drugs in certain patients.
Pharmacokinetic Changes
A. Absorption
There is little
evidence of any major alteration in drug absorption with age. However,
conditions associated with age may alter the rate at which some drugs are
absorbed. Such conditions include altered nutritional habits, greater
consumption of nonprescription drugs (eg, antacids and laxatives), and changes
in gastric emptying, which is often slower in older persons, especially in
older diabetics.
B. Distribution
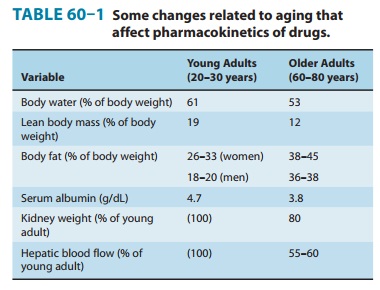
Compared with young
adults, the elderly have reduced lean body mass, reduced body water, and
increased fat as a percentage of body mass. Some of these changes are shown in
Table 60–1. There is usually a decrease in serum albumin, which binds many
drugs, especially weak acids. There may be a concurrent increase in serum orosomucoid (α-acid glycoprotein), a protein that binds many
basic drugs. Thus, the ratio of bound to free drug may be signifi-cantly
altered. As explained, these changes may alter the appropriate loading dose of
a drug. However since both the clearance and the effects of drugs are related
to the free concentra-tion, the steady-state effects of a maintenance dosage
regimen should not be altered by these factors alone. For example, the loading
dose of digoxin in an elderly patient with heart failure should be reduced (if
used at all) because of the decreased apparent volume of distribution. The
maintenance dose may have to be reduced because of reduced clearance of the
drug.
C. Metabolism
The capacity of the
liver to metabolize drugs does not appear to decline consistently with age for
all drugs. Animal studies and some
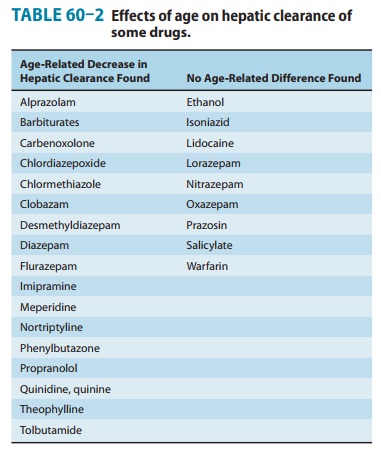
The great-est changes are in phase I reactions, ie, those carried out by microsomal P450 systems. There are much smaller changes in the ability of the liver to carry out conjugation (phase II) reactions . Some of these changes may be caused by decreased liver blood flow (Table 60–1), an important variable in the clearance of drugs that have a high hepatic extraction ratio. In addition, there is a decline with age of the liver’s ability to recover from injury, eg, that caused by alcohol or viral hepatitis.
Therefore, a history of recent liver disease in
an older person should lead to caution in dosing with drugs that are cleared
primarily by the liver, even after apparently complete recovery from the
hepatic insult. Finally, malnutrition and diseases that affect hepatic
function—eg, heart failure—are more common in the elderly. Heart failure may
dramatically alter the abil-ity of the liver to metabolize drugs by reducing
hepatic blood flow. Similarly, severe nutritional deficiencies, which occur more
often in old age, may impair hepatic function.
D. Elimination
Because
the kidney is the major organ for clearance of drugs from the body, the
age-related decline of renal functional capacity is very important. The decline
in creatinine clearance occurs in about two thirds of the population. It is
important to note that this decline is not reflected in an equivalent rise in
serum creati-nine because the production of creatinine is also reduced as
muscle mass declines with age; therefore, serum creatinine alone is not an
adequate measure of renal function. The practical result of this change is
marked prolongation of the half-life of many drugs, and the possibility of
accumulation to toxic levels if dosage is not reduced in size or frequency.
Dosing recommendations for the elderly often include an allowance for reduced renal
clearance. If only the young adult dosage is known for a drug that requires
renal clearance, a rough correction can be made by using the Cockcroft-Gault formula, which is
applicable to patients fromages 40 through 80:
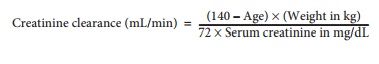
For
women, the result should be multiplied by 0.85 (because of reduced muscle
mass). It must be emphasized that this estimate is, at best, a population estimate and may not apply to
a particular patient. If the patient has normal renal function (up to one third
of elderly patients), a dose corrected on the basis of this estimate will be
too low—but a low dose is initially desirable if one is uncertain of the renal
function in any patient. If a precise measure is needed, a standard 12- or
24-hour creatinine clearance determi-nation should be obtained. As indicated
above, nutritional changes alter pharmacokinetic parameters. A patient who is
severely dehydrated (not uncommon in patients with stroke or other motor
impairment) may have an additional marked reduc-tion in renal drug clearance
that is completely reversible by rehydration.
The
lungs are important for the excretion of volatile drugs. As a result of reduced
respiratory capacity (Figure 60–1) and the increased incidence of active
pulmonary disease in the elderly, the use of inhalation anesthesia is less
common and parenteral agents more common in this age group.
Pharmacodynamic Changes
It
was long believed that geriatric patients were much more “sensitive” to the
action of many drugs, implying a change in the pharmacodynamic interaction of
the drugs with their receptors. It is now recognized that many—perhaps most—of
these appar-ent changes result from altered pharmacokinetics or diminished
homeostatic responses. Clinical studies have supported the idea that the
elderly are more sensitive to some
sedative-hypnotics and analgesics. In addition, some data from animal studies
suggest actual changes with age in the characteristics or numbers of a few
receptors. The most extensive studies suggest a decrease in responsiveness to β-adrenoceptor
agonists. Other examples are discussed below.
Certain
homeostatic control mechanisms appear to be blunted in the elderly. Since
homeostatic responses are often important components of the overall response to
a drug, these physiologic alterations may change the pattern or intensity of
drug response. In the cardiovascular system, the cardiac output increment
required by mild or moderate exercise is successfully provided until at least
age 75 (in individuals without obvious cardiac dis-ease), but the increase is
the result primarily of increased stroke volume in the elderly and not
tachycardia, as in young adults. Average blood pressure goes up with age (in
most Western coun-tries), but the incidence of symptomatic orthostatic
hypotension also increases markedly. It is thus particularly important to check
for orthostatic hypotension on every visit. Similarly, the average 2-hour
postprandial blood glucose level increases by about 1 mg/dL for each year of
age above 50. Temperature regulation is also impaired, and hypothermia is
poorly tolerated by the elderly.
Behavioral & Lifestyle Changes
Major changes in the
conditions of daily life accompany the aging process and have an impact on
health. Some of these (eg, forget-ting to take one’s pills) are the result of
cognitive changes associ-ated with vascular or other pathology. Others relate
to economic stresses associated with greatly reduced income and, possibly,
increased expenses due to illness. One of the most important changes is the
loss of a spouse.
Related Topics