Chapter: Modern Medical Toxicology: Neurotoxic Poisons: Somniferous Drugs
Opium - Somniferous Drugs(Narcotics) Neurotoxic Poisons
SOMNIFEROUS DRUG (NARCOTICS)
Opium
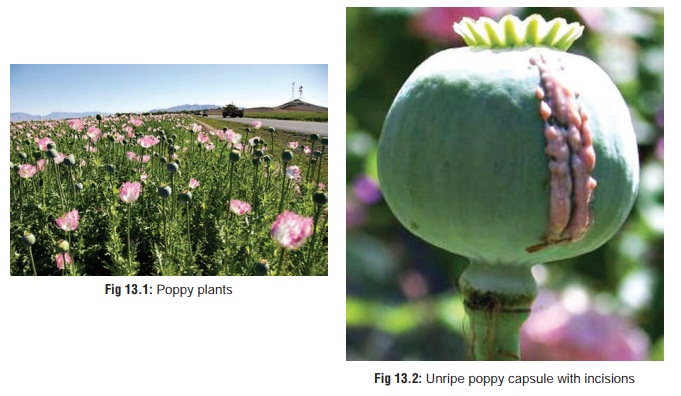
Opium refers to the dried extract of
the poppy plant (Papaversomniferum)
which belongs to the family Papaveraceae.This plant grows well in India, but
its cultivation is banned except on license obtained from the central
government, for growing the plant strictly for the pharmaceutical industry.
Such a license is issued only for the states of Rajasthan, Uttar Pradesh, and Maharashtra.
India produces 70 to 80% of opium that is used worldwide by pharmaceutical
companies to manu-facture several vital drugs including morphine, codeine, and
pethidine. Unfortunately, a significant quantity of opium is funnelled
clandestinely into a global smuggling racket which feeds the illicit drug trade
flourishing in Western countries.
Physical Appearance
·
The poppy plant is a herb growing
upto 1 metre in height (Fig 13.1).
It is minimally branched with leaves clasping
·
the glabrous stem by their cordate
base. The leaves are oblong, irregularly toothed, and slightly sinuate or
lobed.
·
Flowers are large and may be bluish
white, purple, or white in colour.
·
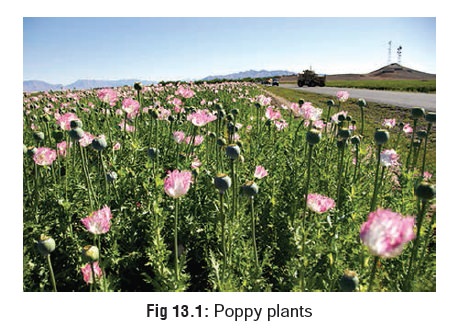
Each plant bears 5 to 8 capsules
which are incised in their unripe state (Fig
13.2) to extract a milky fluid that on drying yields opium.
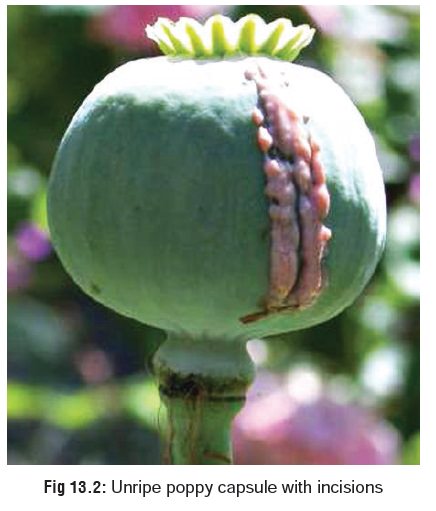
· Crude opium is a dark brown or grey irregular mass (Fig 13.3) with a characteristic odour and bitter taste.
Toxic Part
·
Fruit capsule (unripe).
Toxic Principles
·
Opium obtained from the unripe fruit
capsule contains a number of alkaloids which fall into two groups—
· Phenanthrene group: morphine, codeine, and thebaine.
·
Benzylisoquinoline
group: papaverine and noscapine(narcotine).![]()
Apart
from these natural derivatives there are several other drugs used in
pharmacotherapeutics which are either semisyn-thetic or synthetic analogues.
Examples of other derivatives include alfentanil hydrochloride, alphaprodine,
anileridine hydrochloride, diprenorphine, ethoheptazine, ketobemidone,
meptazinol hydrochloride, methylfentanyl, pholcodine, remifen-tanil hydrochloride,
and sufentanil citrate. When referring to these derivatives, there has always
been confusion in termi-nology. While strictly speaking, the term “opiate”
refers to natural and semisynthetic derivatives, and the term “opioid” is a
more inclusive term applying to all agonists and antagonists with morphine-like
activity, for the sake of convenience (and to avoid confusion),—natural,
semisynthetic, and synthetic.
Uses
·
Opiates have tremendous
pharmacological importance, and are used for various therapeutic purposes (Table 13.1).
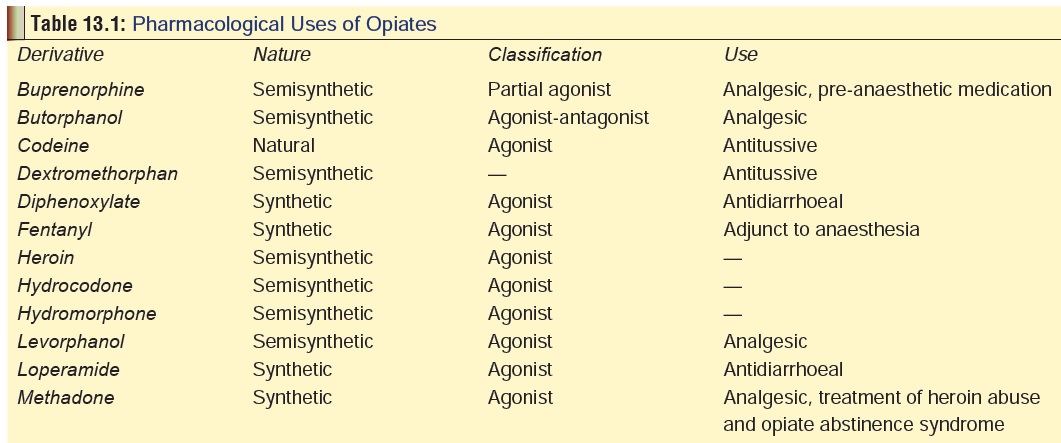
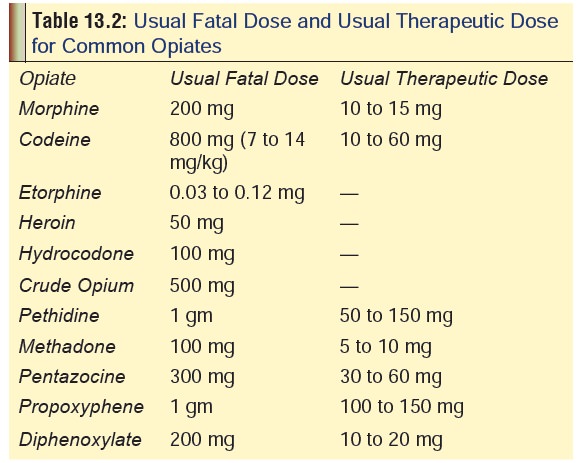
· The usual fatal doses (as well as usual therapeutic doses) of common opiates are listed in Table 13.2.
Mode of Action
There
are three major classes of opiate receptors to which different opiates bind
with differing affinity.
·
The m (mu) receptor is also known as OP3
and consists of 2 sub-types: m1and m2 (OP3A and OP3B).
Most of the clini- cally used opiates are relatively selective for m receptors reflecting their similarity to morphine.
·
The k (kappa) receptor is also known as
OP2 and consists of 3 subtypes: k1, k2, and k3 (OP2A, OP2B,
and OP2C). The d (delta) receptor is also known as
OP1, and is said to be important in spinal and supraspinal
analgesia. Subtypes d1 and d2 have been postulated to exist, but
not confirmed so far.
·
The s (sigma) receptor originally thought
to be an opiate receptor is no longer considered to be opioid in nature since
it is insensitive to naloxone, which is the most important characteristic of
such receptors. However some opiates such as dextromethorphan and pentazocine
are s receptor agonists. Stimulation of s receptor produces psychotomimetic effects and movement
disorders (both of which have been reported with dextromethorphan and
pentazocine).
·
Two more receptors have been postulated to exist, but not demonstrated
so far: e (epsilon) and z (zeta). Mu and delta receptors appear to be involved in
systems that influence mood, reinforcing effects, respiration, pain, blood
pressure, and endocrine and gastrointestinal functions.
·
Kappa receptors are able to produce endocrine changes and
analgesia. In human subjects kappa agonists appear toproduce dysphoria, rather
than euphoria.
·
Respiration, which is controlled mainly through medullary
respiratory centres with peripheral input from chemorecep- tors and other sources,
is affected by opiates which produce inhibition at chemoreceptors via mu
opiates receptors and in the medulla via mu and delta receptors. Tolerance
develops more quickly to euphoria and other effects than to respira-tory
effects.
Toxicokinetics
·
In general, most opiates are readily
absorbed from the GI tract,* and also can be administered by subcutaneous,
intramuscular or intravenous injection. However the effect of an oral dose is
usually much less than that obtained on parenteral administratrion due to
significant first-pass metabolism in the liver. For example, the
bioavailability of oral morphine is only 25%.
·
Extent of protein-binding is
variable depending on the exact nature of the opiate, and varies from 7% for
codeine to 96% for buprenorphine. Morphine displays protein-binding to the
extent of 34%.
·
The major metabolic pathway of
morphine is conjugation with glucuronic acid to produce morphine-6-glucuronide
which is also pharmacologically active. Excretion occurs n the urine as
morphine-3-glucuronide.
·
Duration of action of opiates varies
from 2 hours (pentazo- cine, pethidine) to 4 hours (morphine, codeine, heroin),
to 8 hours (methadone, buprenorphine). Fentanyl, alfentanil, and surfentanil
are ultra-shortacting (few minutes to 1 hour).
Adverse Effects
·
Respiratory depression, vomiting,
vertigo, dysphoria, miosis, constipation, hypotension, urinary retention, and
pruritis are commonly encountered.
·
Pruritus is a common adverse event
following the adminis-tration of opiates, particularly morphine sulfate.
·
Priapism may be induced by opiates
due to their sympa-tholytic actions which may induce an unopposed cholin-ergic
state that could result in Ach-induced vasorelaxation involving NO pathways.
Alpha-blockade has also been postulated as a mechanism. Autonomic system
dysregula-tion appears not to be dose-specific.
Drug Interactions
·
Depressant effect of opiates is
enhanced by alcohol, pheno- thiazines, cyclic antidepressants and Monoamine
oxidase inhibitors (MAOIs).
·
Concomitant administration of
cimetidine can result in mental confusion.
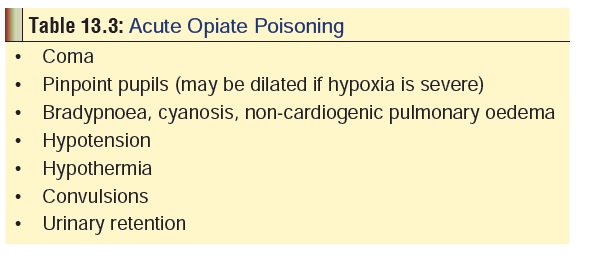
Clinical (Toxic) Features
Acute Poisoning:
·
The triad of coma,
pinpoint pupils, and respiratorydepression
is said to be almost pathognomonic foropiate poisoning. Such cases may be
due to therapeutic overdose, accidental overdose (in addicts), or deliberate
overdose (suicidal). The important clinical manifesta-tions are summarised in Table 13.3.
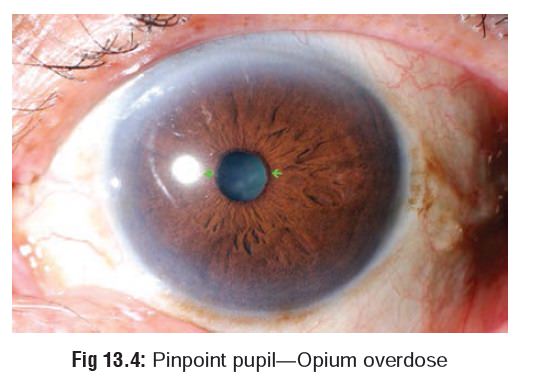
· Pupils are usually pinpoint (Fig 13.4) but may be dilated in the presence of severe acidosis, hypoxia, or respira-tory depression. Pethidine often causes mydriasis.
·
Hypotension may be due to opiate-induced arteriolar and
venous dilation. While bradycardia is said to be common, tachycardia and ECG
readings of sinus tachycardia and nonspecific ST-T segment changes have been
reported.
· Bradypnoea is common in opiate poisoning. Respiratory rates of less than 8/minute are not unusual. Snoring prior to fatal opiate overdose has been reported and is likely due to a failure to maintain the patency of the upper airway. Gurgling may occur due to accumulation of pulmonary oedema fluid. Non-cardiogenic pulmonary oedema (“heroin-lung”) is an infrequent, but severe, complication of heroin overdose and is generally abrupt in onset (immediate-2 hours) following intra-venous heroin overdose. Manifestations include rales, pink frothy sputum, significant hypoxia, and bilateral fluffy infiltrates on chest X-ray. Some patients require mechanical ventilation. Resolution of symptoms usually occurs rapidly with supportive care alone, within hours to 1 to 2 days.
![]()
·
Morphine-induced seizures are primarily seen in neonates.
·
Cramping and constipation as well as sphincter of Oddi spasm
may occur.
·
Hyperkalaemia may occur following an overdose, especially in
the presence of rhabdomyolysis and acute renal failure.
·
Most opiates cross the human placenta. They have been shown
to appear in the foetal circulation within 5 minutes following maternal IV
injection. Morphine appears to act as a vasoconstrictor of the placental
vascu-lature, causing a significant decrease in the biophysical profile score
as a result of absent foetal breathing move-ments and a nonreactive nonstress
test (NST). If delivery occurs quickly following an opiate dose to the mother,
or after adequate time has passed to allow for maternal clearance, it is
unlikely that the foetus would be affected.
Foetuses
demonstrating significant distress and acidosis and whose mothers received
opiates 1 to 3 hours prior to delivery, or multiple doses, may be at increased
risk for respiratory depression, which would most likely be multifactorial in
origin.
Chronic Poisoning:
·
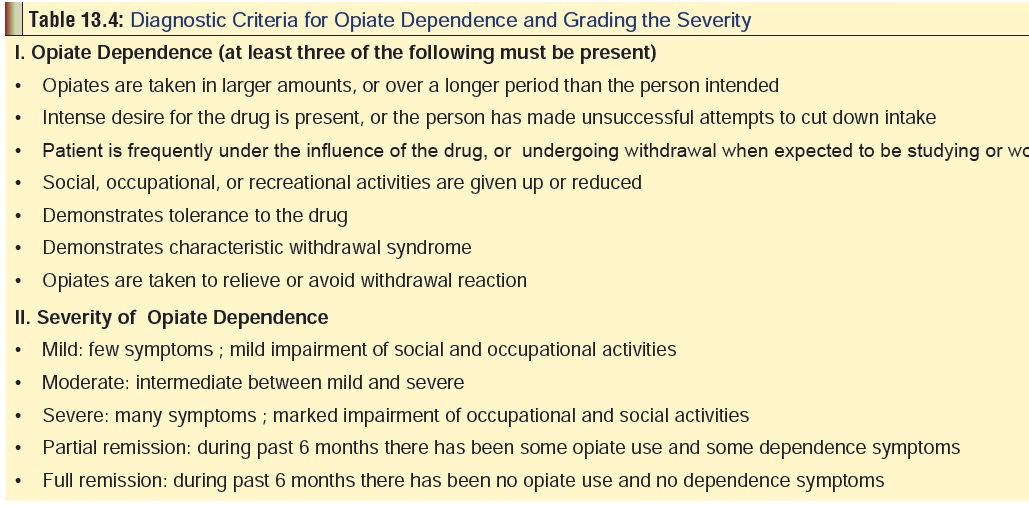
The American Psychiatric Association has laid out diagnostic
criteria for opiate dependence and for catego-rising the severity of such
dependence (Table 13.4).
·
The following are some useful
pointers which indicate opiate addiction:
o Unusual
mood swings, periods of depression alter-nating with euphoria.
o Withdrawal
from family, friends, and social activities. –– Frequent domestic strife.
o Long
hours of unexplained absence from home.
o Unexplained
overspending.
o Frequent
conflicts with law (e.g. driving offences).
o Dwindling
sexual drive.
o Pills,
syringes, etc. lying around the house.
o Bloody
swabs or tissues lying around the home or in the woking place.
o Periodic
disappearances into a locked room (bath- room, bedroom, etc.).
o Pinpoint
pupils.
o Weight
loss, pallor.
o Chronic
constipation.
o Periodic
withdrawal manifestations— sweating, tremors.
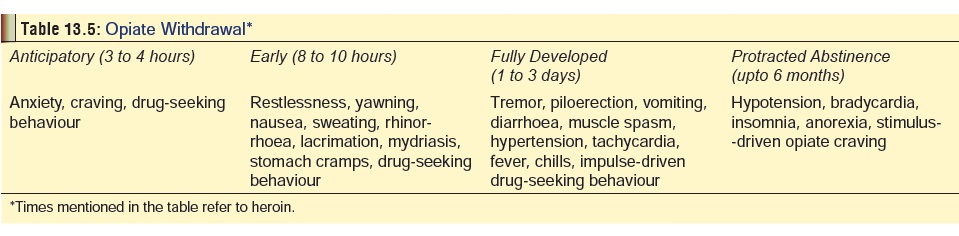
In addition, an addict may have dermal scars (from intra-venous abuse) (Fig 13.5), and suffer from amnesia, confusion, and occasional hallucinations. Compartment syndrome may occur following abuse of narcotic injections, such as heroin.Abrupt cessation of opiate intake can cause a withdrawal reac- tion (cold turkey).* Common manifestations are mentioned in Table 13.5. Neonatal withdrawal may be seen in the infants of addicted mothers 12 to 72 hours after birth. Infants may be dehydrated, irritable, and experience tremors and cry continu- ally and may have diarrhoea.

Related Topics