Chapter: Nutrition and Diet Therapy: Nutritional Care of Clients
Nutritional Care: Feeding the Client

FEEDING THE CLIENT
In the home, the
family menu should serve as the basis of the client’s meal whenever possible.
This usually pleases the client because it makes her or him feel a part of the
family. It also reduces food preparation time and costs.
Family
meals are easily adapted for the client by omitting or adding certain foods or
by varying the method of preparation. Suppose the client was to limit fat
intake and the family menu was the following:
Fried hamburgers
Mashed potatoes with
butter
Buttered peas
Tossed salad with
French dressing
Ice cream with fresh
strawberries
Whole milk
Broiling the hamburgers
for everyone instead of frying would help limit the fat content. The client’s
mashed potatoes might be served with little or no butter, and the peas with
only salt and pepper and perhaps a suitable spice, herb, or lemon. The client
could be served the tossed salad with fat-free dressing and, for dessert,
strawberries with low-fat ice cream. Fat-free milk is a simple substitute for
whole milk.
Serving the Meal
When a meal is served
at the bedside, the tray should be lined with a pretty cloth or paper liner.
Attractive dishes that fit the tray conveniently without crowding it should be
used. The food should be arranged attractively on the plate, with a colorful
garnish such as a slice of fruit, parsley, or vege-table stick. The garnish
must fit into the client’s diet plan, however. Utensils must be arranged
conveniently. Water should be served as well as another beverage (unless it is
prohibited by the physician). Foods must be served at proper temperatures.
When the client is on
complete bed rest, special preparations are required before the meal is served.
The client should be given the opportunity to use the bedpan and to wash before
the meal is served. The room can be ventilated and the bedcovers straightened.
The client should be helped to a comfortable posi-tion, and any unpleasant
sights should be removed before the meal is served. Pleasant conversation
during the preparations can improve the client’s mood considerably. Certain
topics of conversation can help stimulate the client’s interest in eating. The
client might be told that the family is anticipating the same meal. Perhaps the
recipes used will interest some clients. Appropriate remarks on the client’s
progress, whenever possible, are helpful.
When the meal
preparations are complete, the tray should be placed so that it is easy for the
client to feed herself or himself or, if necessary, convenient for someone else
to do the feeding. If the client needs help, the napkin should be opened and
placed, the bread spread, the meat cut, and the straw offered. The client
should be encouraged to eat and be allowed sufficient time. If the meal is
interrupted, the tray should be reheated and served again as soon as the
inter-ruption has resolved.
The tray should be
removed and the client helped to brush her or his teeth when the meal is
finished. The kinds and amounts of food refused, the time, type of diet, and
client’s appetite should be recorded on the client’s chart after each meal. At
times, the provider may request a calorie and protein count, which is an
accurate report of the types and amounts of food eaten.
Feeding the Client Who Requires Assistance
If the client is
unable to feed herself or himself, the person doing the feeding should sit near
the side of the bed (Figure 23-1). Small amounts of food should be placed
toward the back of the mouth with a slight pressure on the tongue with the
spoon or fork. Clients should not be fed with a syringe. If the client is
suffering from one-sided paralysis, the food and drinking straw must be placed
in the nonparalyzed side of the mouth. The client must be allowed to help
herself or himself as much as possible. If the client begins to choke, help her
or him sit up straight. Do not give food or water while the client is choking.
The client’s mouth should be wiped as needed. A client diagnosed with dysphagia
will require a specialized diet. Depending upon the swallowing abnormality, the
client may need pureed foods with either thin or thickened (to a nectar or
honey consistency) liquids. A dysphagic client should not use straws.

Feeding the Blind Client
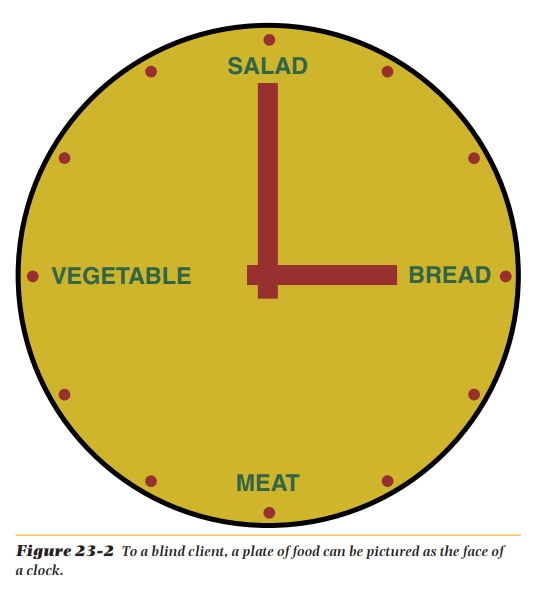
Special care must be
taken in serving a meal to a client who is blind. An appe-tizing description of
the meal can help create a desire to eat. To help the client who is blind feed
herself or himself, arrange the food as if the plate were the face of a clock
(Figure 23-2). The meat might be put at 6 o’clock, vegetables at 9 o’clock,
salad at 12, and bread at 3 o’clock. The person who regularly arranges the meal
should remember to use the same pattern for all meals. People who are blind
usually feel better when they can help themselves.
Related Topics