Chapter: Clinical Pharmacology: Neurologic and neuromuscular drugs
Neuromuscular blocking drugs
Neuromuscular blocking drugs
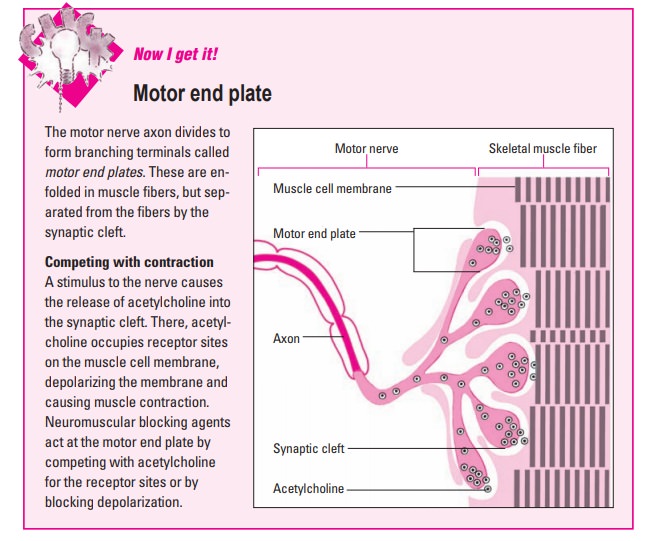
Neuromuscular blocking
drugs relax skeletal
muscles by disrupt-ing the transmission of nerve impulses at the motor end
plate (the branching terminals of a motor nerve axon). (See Motor end plate)
Neuromuscular blockers have three major clinical
indications:
·
to relax skeletal muscles during surgery
· to reduce the intensity of muscle spasms in drug- or electri-cally induced seizures
·
to manage patients who are fighting the use of a ventilator to help with
breathing.
Two main classifications
There are two main classes of natural and synthetic
drugs used as neuromuscular blockers—nondepolarizing and depolarizing.
Nondepolarizing blocking drugs
Nondepolarizing blocking
drugs, also called competitive or stabi-lizing drugs, are derived from curare alkaloids and
syntheticallysimilar compounds. They include:
·
atracurium
·
cisatracurium
·
pancuronium
·
rocuronium
·
vecuronium.
Pharmacokinetics
Because nondepolarizing blockers are absorbed
poorly from the GI tract, they’re administered parenterally. The I.V. route is
pre-ferred because the action is more predictable.
Distribution
These drugs are distributed rapidly throughout the
body.
Metabolism and excretion
A variable but large proportion of the
nondepolarizing drugs is ex-creted unchanged in urine. Some drugs, such as
atracurium, pan-curonium, and vecuronium, are partially metabolized in the
liver.
Pharmacodynamics
Nondepolarizing blockers compete with acetylcholine
at the cholinergic receptor sites of the skeletal muscle membrane. This blocks
acetylcholine’s neurotransmitter action, preventing the muscle from
contracting.
The effect can be counteracted by
anticholinesterase drugs, such as neostigmine and pyridostigmine, which inhibit
the action of acetylcholinesterase, the enzyme that destroys acetylcholine.
From weakness to paralysis
The initial muscle weakness produced by these drugs
quickly changes to a flaccid (loss of muscle tone) paralysis that affects the
muscles in a specific sequence. The first muscles to exhibit flaccid paralysis
are those of the eyes, face, and neck. Next, the limb, ab-domen, and trunk
muscles become flaccid.
Lastly, the intercostal muscles (between the ribs)
and diaphragm (the breathing muscle) are paralyzed. Recovery from the paralysis
usually occurs in the reverse order.
Conscious and aware
Because these drugs don’t cross the blood-brain
barrier, the patient remains conscious and can feel pain. Even though the
patient is paralyzed, he’s aware of what’s happening to him and can experience
extreme anxi-ety but can’t communicate his feelings.
For this reason, an analgesic or antianxi-ety drug
should be administered along with a neuromuscular blocker. (See Us-ing a neuromuscular blocker safely.)
Pharmacotherapeutics
Nondepolarizing blockers are used for intermediate
or prolonged muscle relaxation to:
·
ease the passage of an endotracheal (ET) tube
·
decrease the amount of anesthetic required during surgery
·
facilitate realignment of broken bones and dislocated joints
·
paralyze patients who need ventilatory support but who fight the ET tube
and ventilation
·
prevent muscle injury during electroconvulsive therapy (ECT) (passing an
electric current through the brain to treat depression) by reducing the
intensity of muscle spasms.
Drug interactions
These drugs alter the effects of nondepolarizing
neuromuscular blockers:
o
Aminoglycoside antibiotics and anesthetics potentiate or exag-gerate the
neuromuscular blockade.
·
Drugs that alter the serum levels of the electrolytes calcium,
magnesium, or potassium also alter the effects of the nondepolar-izing
blockers.
·
The anticholinesterases (neostigmine, pyridostigmine, and edro-phonium)
antagonize nondepolarizing blockers and are used as antidotes to them.
·
Drugs that can increase the intensity and duration of paralysis when
taken with a nondepolarizing blocker include inhalation anesthetics,
aminoglycosides, clindamycin, polymyxin, verapamil, quinine derivatives,
ketamine, lithium, nitrates, thiazide diuretics, tetracyclines, and magnesium
salts.
· Drugs that can cause decreased neuromuscular blockade when taken with a
nondepolarizing blocker include carbamazepine, hy-dantoins, ranitidine, and
theophylline. (See Adverse reactions
tonondepolarizing blockers.)
o
Concurrent use of corticosteroids may result in prolonged mus-cle
weakness.
Depolarizing blocking drugs
Succinylcholine is the only therapeutic depolarizing blockingdrug.
Although it’s similar to the nondepolarizing blockers in its therapeutic
effect, its mechanism of action differs. Succinyl-choline acts like
acetylcholine, but it isn’t inactivated by cholinesterase. It’s the drug of
choice when short-term muscle re-laxation is needed.
Pharmacokinetics
Because succinylcholine is absorbed poorly from the
GI tract, the preferred administration route is I.V.; the I.M. route can be
used, if necessary.
Metabolism and excretion
Succinylcholine is hydrolyzed in the liver and
plasma by the en-zyme pseudocholinesterase, producing a metabolite with a
nonde-polarizing blocking action. Succinylcholine is excreted by the kid-neys,
with a small amount excreted unchanged.
Pharmacodynamics
After administration, succinylcholine is rapidly
metabolized, but at a slower rate than acetylcholine. As a result,
succinylcholine re-mains attached to receptor sites on the skeletal muscle
membrane for a longer period of time. This prevents repolarization of the
mo-tor end plate and results in muscle paralysis.
Pharmacotherapeutics
Succinylcholine is the drug of choice for
short-term muscle relax-ation, such as during intubation and ECT.
Drug interactions
The action of succinylcholine is potentiated by a
number of anes-thetics and antibiotics. In contrast to their interaction with
nonde-polarizing blockers, anticholinesterases increase succinylcholine
blockade. (See Adverse reactions to
succinylcholine.)
Related Topics