Chapter: Obstetrics and Gynecology: Multifetal Gestation
Multifetal Gestation: Diagnosis and Antenatal Management
DIAGNOSIS AND ANTENATAL MANAGEMENT
Most multifetal pregnancies are
diagnosed using ultrasound.
On a
clinical basis, twin pregnancy should be suspected when the uterine size is
large for the calculated gestational age.
A difference of 4 cm or more
between the weeks of gesta-tion and the measured fundal height should prompt
eval-uation with ultrasound to detect the cause (e.g., inaccurate gestational
age, multiple gestation, hydramnios, gesta-tional trophoblastic disease, or
pelvic tumor).
Serial ultrasound assessments
have shown that only 50% of twin pregnancies detected in the first trimester
result in the delivery of viable twins. The other 50% of cases deliver a single
fetus because of intrauterine demise and ultimate resorption of one embryo/fetus
(vanishing twin syndrome). During the first ultrasonographic exam-ination that
confirms a twin gestation, chorionicity should be determined because the
potential morbidity and mor-tality associated with a monochorionic gestation is
differ-ent from that of a dichorionic gestation (described below). Chorionicity
can be determined with almost 100% cer-tainty as early as 9 to 10 weeks of
gestational age.
Once the diagnosis of twin
pregnancy has been made and chorionicity has been assigned, subsequent
antenatal care addresses each of the potential concerns for mother and fetus,
as listed in Table 17.2. Although the maternal blood volume is greater with a
twin gestation than with a singleton pregnancy, the anticipated blood loss at
delivery is also greater. Anemia is more common in these patients, and a
balanced diet during pregnancy, which may include increased intake of iron,
folate, and other micronutrients, is important. Because of the increased risk for preterm labor inmultiple gestations,
careful attention to detection of uterine con-tractions is important, and the
patient should be cautioned about signs and symptoms of preterm labor, such as
low back pain, a thin or increase in vaginal discharge, and vaginal bleeding. Cervical
examinations to detect early effacement and dila-tion are often done every 1 to
2 weeks beginning in the midtrimester. When available, serial ultrasound
assess-ments of endovaginal cervical length may be interspersed with the
vaginal examinations.
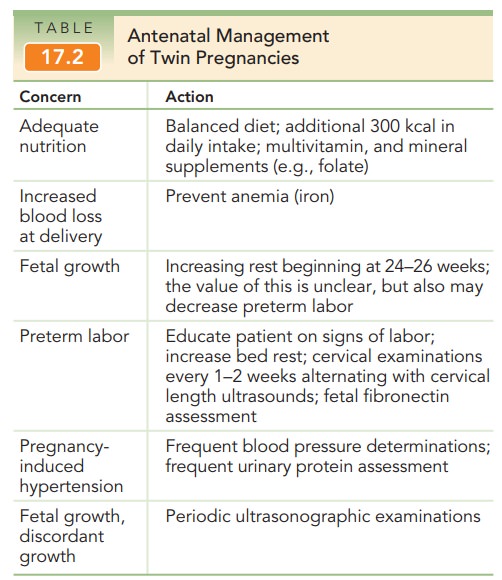
Assessment of fetal fibronectin may aid in predicting preterm delivery in women, but it has limited predictive value in multifetal gestations.
At each visit, blood pressure should be evaluated and, if elevated, urine
protein should be assessed. Beginning at 30 to 32 weeks, daily fetal kick
counts are usually begun to help assess fetal well-being.
With
multifetal gestations, periodic ultrasonographic exam-ination should be
performed approximately every 4 weeks, begin-ning at 16 to 18 weeks of
gestation. At each examination,growth of each fetus is
assessed and an estimate of amniotic fluid volume is made. Discordant growth is
defined as a 15% to 25% reduction in the estimated fetal weight of the
small-est fetus compared with the largest. Ultrasonography should be performed
more often in cases of discordant growth.
Related Topics