Chapter: Medical Physiology: Female Physiology Before Pregnancy and Female Hormones
Monthly Ovarian Cycle; Function of the Gonadotropic Hormones
Monthly Ovarian Cycle; Function of the Gonadotropic Hormones
The normal reproductive years of the female are characterized by monthly rhythmical changes in the rates of secretion of the female hormones and correspon-ding physical changes in the ovaries and other sexual organs. This rhythmical pattern is called the femalemonthly sexual cycle (or, less accurately, the menstrual cycle). The duration of the cycle averages 28 days. Itmay be as short as 20 days or as long as 45 days in some women, although abnormal cycle length is frequently associated with decreased fertility.
There are two significant results of the female sexual cycle. First, only a single ovum is normally released from the ovaries each month, so that normally only a single fetus will begin to grow at a time. Second, the uterine endometrium is prepared in advance for implantation of the fertilized ovum at the required time of the month.
Gonadotropic Hormones and Their Effects on the Ovaries
The ovarian changes that occur during the sexual cycle depend completely on the gonadotropic hormones FSH and LH, secreted by the anterior pituitary gland.In the absence of these hormones, the ovaries remain inactive, which is the case throughout childhood, when almost no pituitary gonadotropic hormones are secreted. At age 9 to 12 years, the pituitary begins to secrete progressively more FSH and LH, which leads to onset of normal monthly sexual cycles beginning between the ages of 11 and 15 years. This period of change is called puberty, and the time of the first men-strual cycle is called menarche. Both FSH and LH are small glycoproteins having molecular weights of about 30,000.
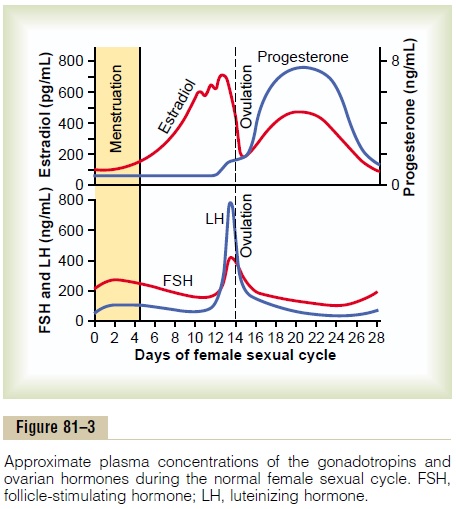
During each month of the female sexual cycle, there is a cyclical increase and decrease of both FSH and LH, as shown in the bottom of Figure 81–3. These cyclical variations cause cyclical ovarian changes, which are explained in the following sections.
Both FSH and LH stimulate their ovarian target cells by combining with highly specific FSH and LH receptors in the ovarian target cell membranes. In turn, the activated receptors increase the cells’ rates of secretion and usually the growth and proliferation of the cells as well. Almost all these stimulatory effects result from activation of the cyclic adenosinemonophosphate second messenger system in the cellcytoplasm, which causes the formation of proteinkinase and multiple phosphorylations of key enzymes that stimulate sex hormone synthesis.
Ovarian Follicle Growth— “Follicular” Phase of the Ovarian Cycle
Figure 81–4 shows the progressive stages of follicular growth in the ovaries. When a female child is born, each ovum is surrounded by a single layer of granu-losa cells; the ovum, with this granulosa cell sheath, is called a primordial follicle, as shown in the figure. Throughout childhood, the granulosa cells are believed to provide nourishment for the ovum and to secrete an oocyte maturation-inhibiting factor that keeps the ovum suspended in its primordial state in the prophase stage of meiotic division. Then, after puberty, when FSH and LH from the anterior pituitary gland begin to be secreted in significant quantities, the ovaries, together with some of the follicles within them, begin to grow.
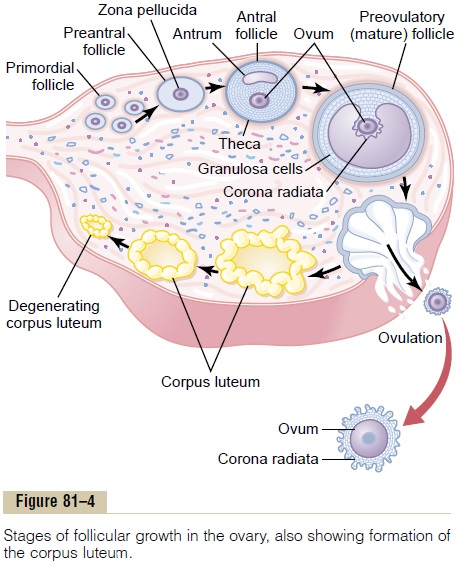
The first stage of follicular growth is moderate enlargement of the ovum itself, which increases in diameter twofold to threefold. Then follows growth of additional layers of granulosa cells in some of the fol-licles; these follicles are known as primary follicles.
Development of Antral and Vesicular Follicles. During thefirst few days of each monthly female sexual cycle, the concentrations of both FSH and LH secreted by the anterior pituitary gland increase slightly to mod-erately, with the increase in FSH slightly greater than that of LH and preceding it by a few days. These hor-mones, especially FSH, cause accelerated growth of 6 to 12 primary follicles each month. The initial effect is rapid proliferation of the granulosa cells, giving rise to many more layers of these cells. In addition, spindle cells derived from the ovary interstitium collect in several layers outside the granulosa cells, giving rise to a second mass of cells called the theca. This is divided into two layers. In the theca interna, the cells take on epithelioid characteristics similar to those of the gran-ulosa cells and develop the ability to secrete additional steroid sex hormones (estrogen and progesterone).
The outer layer, the theca externa, develops into a highly vascular connective tissue capsule that becomes the capsule of the developing follicle.
After the early proliferative phase of growth, lasting for a few days, the mass of granulosa cells secretes a follicular fluid that contains a high concentration ofestrogen, one of the important female sex hormones (discussed later). Accumulation of this fluid causes an antrum to appear within the mass of granulosa cells, asshown in Figure 81–4.
The early growth of the primary follicle up to the antral stage is stimulated mainly by FSH alone. Then greatly accelerated growth occurs, leading to still larger follicles called vesicular follicles. This acceler-ated growth is caused by the following: (1) Estrogen is secreted into the follicle and causes the granulosa cells to form increasing numbers of FSH receptors; this causes a positive feedback effect, because it makes the granulosa cells even more sensitive to FSH. (2) The pituitary FSH and the estrogens combine to promote LH receptors on the original granulosa cells, thus allowing LH stimulation to occur in addition to FSH stimulation and creating an even more rapid increase in follicular secretion. (3) The increasing estrogens from the follicle plus the increasing LH from the ante-rior pituitary gland act together to cause proliferation of the follicular thecal cells and increase their secre-tion as well.
Once the antral follicles begin to grow, their growth occurs almost explosively. The ovum itself also enlarges in diameter another threefold to four-fold, giving a total ovum diameter increase up to 10-fold, or a mass increase of 1000-fold. As the follicle enlarges, the ovum itself remains embedded in a mass of granulosa cells located at one pole of the follicle.
Only One Follicle Fully Matures Each Month, and the Remain-der Undergo Atresia. After a week or more of growth—but before ovulation occurs—one of the follicles begins to outgrow all the others; the remaining 5 to 11 developing follicles involute (a process called atresia), and these follicles are said to become atretic.
The cause of the atresia is unknown, but it has been postulated to be the following: The large amounts of estrogen from the most rapidly growing follicle act on the hypothalamus to depress further enhancement of FSH secretion by the anterior pituitary gland, in this way blocking further growth of the less well developed follicles. Therefore, the largest follicle continues to grow because of its intrinsic positive feedback effects, while all the other follicles stop growing and actually involute.
This process of atresia is important, because it nor-mally allows only one of the follicles to grow large enough each month to ovulate; this usually prevents more than one child from developing with each preg-nancy. The single follicle reaches a diameter of 1 to 1.5 centimeters at the time of ovulation and is called the mature follicle.
Ovulation
Ovulation in a woman who has a normal 28-day female sexual cycle occurs 14 days after the onset of menstruation. Shortly before ovulation, the protruding outer wall of the follicle swells rapidly, and a small area in the center of the follicular capsule, called the stigma, protrudes like a nipple. In another 30 minutes or so, fluid begins to ooze from the follicle through the stigma, and about 2 minutes later, the stigma ruptures widely, allowing a more viscous fluid, which has occupied the central portion of the follicle, to evagi-nate outward. This viscous fluid carries with it the ovum surrounded by a mass of several thousand small granulosa cells, called the corona radiata.
Surge of LH Is Necessary for Ovulation. LH is necessaryfor final follicular growth and ovulation. Without this hormone, even when large quantities of FSH are available, the follicle will not progress to the stage of ovulation.
About 2 days before ovulation, the rate of secretion of LH by the anterior pituitary gland increases markedly, rising 6- to 10-fold and peaking about 16 hours before ovulation. FSH also increases about 2-fold to 3-fold at the same time, and the FSH and LH act synergistically to cause rapid swelling of the follicle during the last few days before ovulation. The LH also has a specific effect on the granulosa and theca cells, converting them mainly to progesterone-secreting cells. There-fore, the rate of secretion of estrogen begins to fall about 1 day before ovulation, while increasing amounts of progesterone begin to be secreted.
It is in this environment of (1) rapid growth of the follicle, (2) diminishing estrogen secretion after a pro-longed phase of excessive estrogen secretion, and (3) initiation of secretion of progesterone that ovulation occurs. Without the initial preovulatory surge of LH, ovulation will not take place.
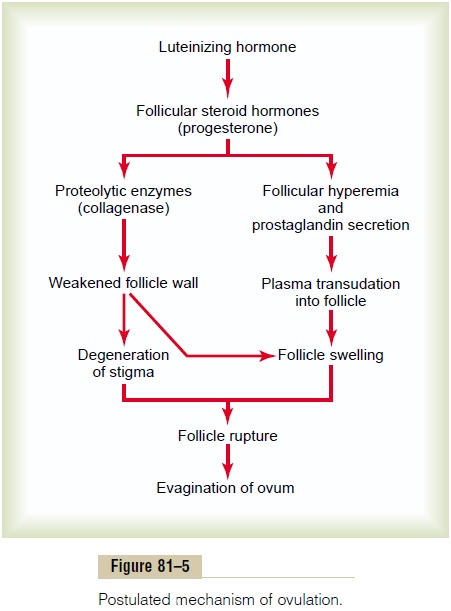
Initiation of Ovulation. Figure 81–5 gives a schema for theinitiation of ovulation, showing the role of the large quantity of LH secreted by the anterior pituitary gland. This LH causes rapid secretion of follicular steroid hormones that contain progesterone. Within a few hours, two events occur, both of which are neces-sary for ovulation: (1) The theca externa (the capsule of the follicle) begins to release proteolytic enzymes from lysosomes, and these cause dissolution of the fol-licular capsular wall and consequent weakening of the wall, resulting in further swelling of the entire follicle and degeneration of the stigma. (2) Simultaneously, there is rapid growth of new blood vessels into the fol-licle wall, and at the same time, prostaglandins (local hormones that cause vasodilation) are secreted into the follicular tissues. These two effects cause plasma transudation into the follicle, which contributes to follicle swelling. Finally, the combination of follicle swelling and simultaneous degeneration of the stigma causes follicle rupture, with discharge of the ovum.
Corpus Luteum—“Luteal” Phase of the Ovarian Cycle
During the first few hours after expulsion of the ovum from the follicle, the remaining granulosa and theca interna cells change rapidly into lutein cells. They enlarge in diameter two or more times and become filled with lipid inclusions that give them a yellowish appearance.This process is calledluteinization, and the total mass of cells together is called the corpus luteum, which is shown in Figure 81–4. A well-developed vascular supply also grows into the corpus luteum.
The granulosa cells in the corpus luteum develop extensive intracellular smooth endoplasmic reticula that form large amounts of the female sex hormones progesterone and estrogen (more progesterone thanestrogen). The theca cells form mainly the androgens androstenedione and testosteronerather than femalesex hormones. However, most of these hormones are also converted by the granulosa cells into the female hormones.
In the normal female, the corpus luteum grows to about 1.5 centimeters in diameter, reaching this stage of development 7 to 8 days after ovulation. Then it begins to involute and eventually loses its secretory function as well as its yellowish, lipid characteristic about 12 days after ovulation, becoming the corpusalbicans; during the ensuing few weeks, this is replacedby connective tissue and over months is absorbed.
Luteinizing Function of LH. The change of granulosa andtheca interna cells into lutein cells is dependent mainly on LH secreted by the anterior pituitary gland. In fact, this function gives LH its name—“luteinizing,” for “yellowing.” Luteinization also depends on extrusion of the ovum from the follicle. A yet uncharacterized local hormone in the follicular fluid, called luteiniza-tion-inhibiting factor, seems to hold the luteinizationprocess in check until after ovulation.
Secretion by the Corpus Luteum: An Additional Function of LH.
The corpus luteum is a highly secretory organ, secret-ing large amounts of both progesterone and estrogen. Once LH (mainly that secreted during the ovulatory surge) has acted on the granulosa and theca cells to cause luteinization, the newly formed lutein cells seem to be programmed to go through a preordained sequence of (1) proliferation, (2) enlargement, and (3) secretion, followed by (4) degeneration. All this occurs in about 12 days. We shall see in the discussion of pregnancy that another hormone with almost exactly the same properties as LH, chorionicgonadotropin, which is secreted by the placenta, canact on the corpus luteum to prolong its life—usually maintaining it for at least the first 2 to 4 months of pregnancy.
Involution of the Corpus Luteum and Onset of the Next Ovarian
Cycle. Estrogen in particular and progesterone to alesser extent, secreted by the corpus luteum during the luteal phase of the ovarian cycle, have strong feedback effects on the anterior pituitary gland to maintain low secretory rates of both FSH and LH.
In addition, the lutein cells secrete small amounts of the hormone inhibin, the same as the inhibin secreted by the Sertoli cells of the male testes. This hormone inhibits secretion by the anterior pituitary gland, espe-cially FSH secretion. Low blood concentrations of both FSH and LH result, and loss of these hormones finally causes the corpus luteum to degenerate completely, a process called involution of the corpus luteum.
Final involution normally occurs at the end of almost exactly 12 days of corpus luteum life, which is around the 26th day of the normal female sexual cycle, 2 days before menstruation begins. At this time, the sudden cessation of secretion of estrogen, proges-terone, and inhibin by the corpus luteum removes the feedback inhibition of the anterior pituitary gland, allowing it to begin secreting increasing amounts of FSH and LH again. FSH and LH initiate the growth of new follicles, beginning a new ovarian cycle. The paucity of secretion of progesterone and estrogen at this time also leads to menstruation by the uterus, as explained later.
Summary
About every 28 days, gonadotropic hormones from the anterior pituitary gland cause about 8 to 12 new folli-cles to begin to grow in the ovaries. One of these fol-licles finally becomes “mature” and ovulates on the 14th day of the cycle. During growth of the follicles, mainly estrogen is secreted.
After ovulation, the secretory cells of the ovulating follicle develop into a corpus luteum that secretes large quantities of both the major female hormones, progesterone and estrogen. After another 2 weeks, the corpus luteum degenerates, whereupon the ovarian hormones estrogen and progesterone decrease greatly, and menstruation begins. A new ovarian cycle then follows.
Related Topics