Chapter: Medical Physiology: Female Physiology Before Pregnancy and Female Hormones
Corpus Luteum-ÔÇťLutealÔÇŁ Phase of the Ovarian Cycle
Corpus Luteum-ÔÇťLutealÔÇŁ Phase of the Ovarian Cycle
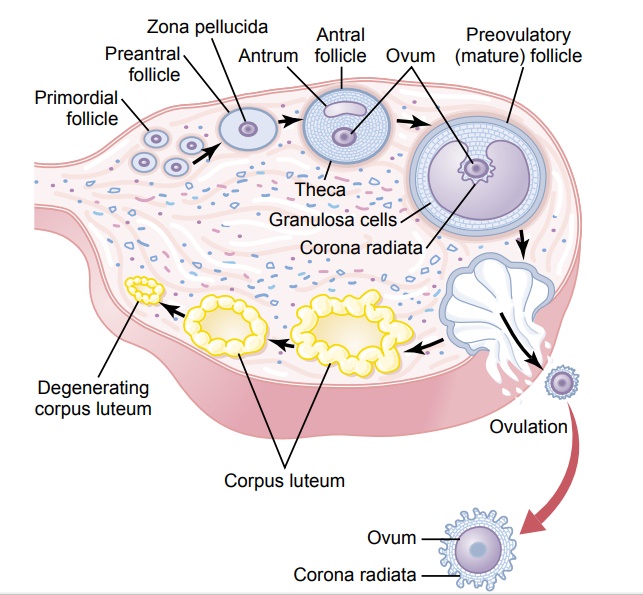
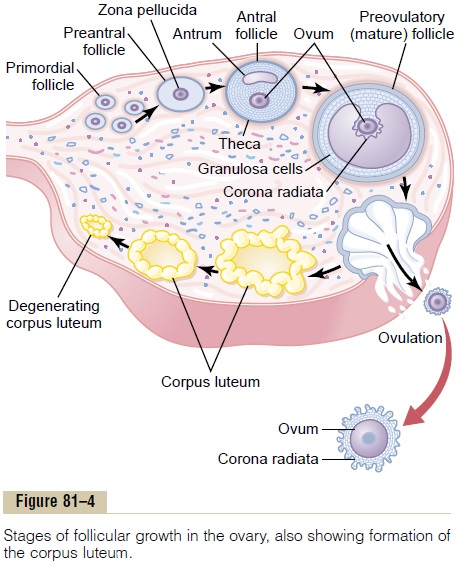
During the first few hours after expulsion of the ovum from the follicle, the remaining granulosa and theca interna cells change rapidly into lutein cells. They enlarge in diameter two or more times and become filled with lipid inclusions that give them a yellowish appearance.This process is called luteinization, and the total mass of cells together is called the corpus luteum, which is shown in Figure 81ÔÇô4. A well-developed vascular supply also grows into the corpus luteum.
The granulosa cells in the corpus luteum develop extensive intracellular smooth endoplasmic reticula that form large amounts of the female sex hormones progesterone and estrogen (more progesterone thanestrogen). The theca cells form mainly the androgensandrostenedione and testosterone rather than femalesex hormones. However, most of these hormones are also converted by the granulosa cells into the female hormones.
In the normal female, the corpus luteum grows to about 1.5 centimeters in diameter, reaching this stage of development 7 to 8 days after ovulation. Then it begins to involute and eventually loses its secretory function as well as its yellowish, lipid characteristic about 12 days after ovulation, becoming the corpusalbicans; during the ensuing few weeks, this is replacedby connective tissue and over months is absorbed.
Luteinizing Function of LH. The change of granulosa andtheca interna cells into lutein cells is dependent mainly on LH secreted by the anterior pituitary gland. In fact, this function gives LH its nameÔÇöÔÇťluteinizing,ÔÇŁ for ÔÇťyellowing.ÔÇŁ Luteinization also depends on extrusion of the ovum from the follicle. A yet uncharacterized local hormone in the follicular fluid, called luteiniza-tion-inhibiting factor, seems to hold the luteinizationprocess in check until after ovulation.
Secretion by the Corpus Luteum: An Additional Function of LH.
The corpus luteum is a highly secretory organ, secret-ing large amounts of both progesterone and estrogen. Once LH (mainly that secreted during the ovulatory surge) has acted on the granulosa and theca cells to cause luteinization, the newly formed lutein cells seem to be programmed to go through a preordained sequence of (1) proliferation, (2) enlargement, and (3) secretion, followed by (4) degeneration. All this occurs in about 12 days. We shall see in the discussion of pregnancy that another hormone with almost exactly the same properties as LH, chorionicgonadotropin, which is secreted by the placenta, canact on the corpus luteum to prolong its lifeÔÇöusually maintaining it for at least the first 2 to 4 months of pregnancy.
Involution of the Corpus Luteum and Onset of the Next Ovarian
Cycle. Estrogen in particular and progesterone to alesser extent, secreted by the corpus luteum during the luteal phase of the ovarian cycle, have strong feedback effects on the anterior pituitary gland to maintain low secretory rates of both FSH and LH.
In addition, the lutein cells secrete small amounts of the hormone inhibin, the same as the inhibin secreted by the Sertoli cells of the male testes. This hormone inhibits secretion by the anterior pituitary gland, espe-cially FSH secretion. Low blood concentrations of both FSH and LH result, and loss of these hormones finally causes the corpus luteum to degenerate completely, a process calledinvolution of the corpus luteum.
Final involution normally occurs at the end of almost exactly 12 days of corpus luteum life, which is around the 26th day of the normal female sexual cycle, 2 days before menstruation begins. At this time, the sudden cessation of secretion of estrogen, proges-terone, and inhibin by the corpus luteum removes the feedback inhibition of the anterior pituitary gland, allowing it to begin secreting increasing amounts of FSH and LH again. FSH and LH initiate the growth of new follicles, beginning a new ovarian cycle. The paucity of secretion of progesterone and estrogen at this time also leads to menstruation by the uterus, as explained later.
Related Topics